Antigens on the surface of one’s red blood cells determine their blood group. Some people do not contain prevalent antigens, making their blood group rare.
Image credit:© iStock.com, Md Saiful Islam Khan
In 2011, a woman from the French overseas region of Guadeloupe underwent routine tests before a surgery. Strikingly, doctors could not identify her blood group, which was so unique that they did not find any matches even from her family.1
Halfway across the world in India, doctors recently faced a similar challenge upon testing a woman’s blood before she underwent a surgery.2 Although tests revealed that her blood group was O positive, none of the donor samples were compatible with her blood.
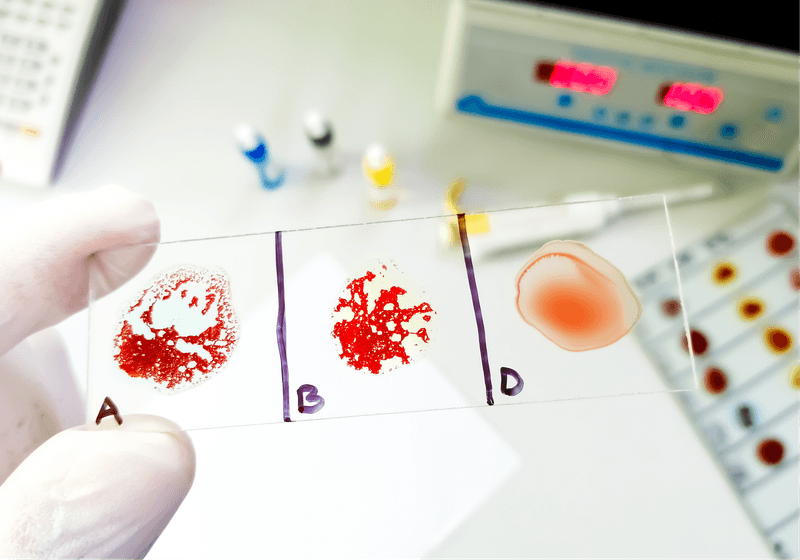
A person’s blood group is determined by the antigens they carry on their red blood cell (RBC) surface. The most familiar blood groups—A, B, and O—stem from the commonly found A and B antigens, while the Rhesus factor dictates Rh-positive or -negative blood groups.3,4 However, these are just two of the common blood group systems and some of the many antigens that influence blood grouping in individuals.

Martin Olsson, a transfusion medicine researcher at Lund University, works to make sure that blood transfusions, stem cell transplants, and organ transplants are matched correctly between donors and recipients. His team also explores the possibility of developing universally-compatible blood.
Roger Lundholm
“In total, there are almost 400 different blood group antigens,” said Martin Olsson, a transfusion medicine researcher at Lund University. “In general, [one has a rare blood group when] that patient…lacks a high frequency antigen.”
Analyzing the DNA of the Indian woman revealed that she carried a genetic variant resulting in the loss of a commonly found Cromer antigen on her RBCs. The patient from Guadeloupe similarly lacked the prevalent Emm antigen on her RBCs.5
While the absence of some other Cromer antigens has been reported previously, the Guadeloupean woman is the only person in the world known so far to carry a blood type without the Emm antigen, leading to the recognition of a 48th blood group: While her blood group is Gwada-negative, that of all the potential donors tested is Gwada-positive.
Olsson and others in the field employ a suite of genomic and molecular techniques to identify and characterize the antigens underlying rare blood types. This not only unravels deeper insights into the biology of blood groups but can also help screen other people with possible rare blood types, setting them up as potential donors.
How Do People with Rare Blood Groups Get Transfusions?
A person’s immune system recognizes their own antigens as “self.” However, receiving blood containing unfamiliar antigens results in the body treating them as invaders and mounting an immune response, including developing antibodies against the foreign antigens.6
As such, a person whose RBCs do not carry a particular antigen would need blood from a donor who also lacks the same antigen. Several hospitals across the world are equipped with a database describing potential donors with rare blood types.
However, both the Indian and Guadeloupean women are the only known people with their respective blood types on the planet so far: They are only compatible with themselves. “This is an absolutely exceptional case,” said Olsson, referring to the findings from the Guadeloupean patient. “My prediction is that there are other people out there with the same blood group…but we certainly haven’t found them yet.”
Until that happens, Olsson said that doctors may need to treat the patients with supplements to boost their hemoglobin levels so that they can donate their own blood. This blood could be stored and used for an autologous transfusion if the need arises.
Studying Rare Blood Groups
In Nobel Prize-winning work, Karl Landsteiner discovered the ABO blood group system by studying the blood of his staff.7 Almost 40 years later, scientists discovered the Rhesus factor when a woman suffered an adverse reaction even though she received her husband’s ABO compatible blood.8 This revealed that more antigens were involved in blood group classification. Eventually, scientists identified other antigens that contributed to various blood types in people.
“Forty years ago, we knew lots of blood groups, but we did not know what molecules—proteins or carbohydrates—the red [blood] cell surface carried to display to the [transfusion recipient’s] immune system,” said Olsson, whose team has established six blood group systems. “And that also meant we didn’t know what genes were responsible for them.”
This prompted Olsson and other scientists in the field to unravel the genetic and molecular basis of almost all blood groups. They subject the DNA of people with rare blood groups to a variety of methods including next-generation sequencing to identify genetic variants that could potentially contribute to the trait.9,10
“You may think, ‘Oh, this is quite academic, and it’s experimental. It’s genes and molecules,’” said Olsson. “But by finding [the variants], we can then screen to find the rare donors. They are out there.”