Hariharan, S., Israni, A. K. & Danovitch, G. Long-term survival after kidney transplantation. N. Engl. J. Med. 385, 729–743 (2021).
Himmelfarb, J., Vanholder, R., Mehrotra, R. & Tonelli, M. The current and future landscape of dialysis. Nat. Rev. Nephrol. 16, 573–585 (2020).
Thurlow, J. S. et al. Global epidemiology of end-stage kidney disease and disparities in kidney replacement therapy. Am. J. Nephrol. 52, 98–107 (2021).
Harris, D. C. H. et al. Increasing access to integrated ESKD care as part of universal health coverage. Kidney Int. 95, S1–S33 (2019).
Francis, A. et al. Chronic kidney disease and the global public health agenda: an international consensus. Nat. Rev. Nephrol. 20, 473–485 (2024).
Liyanage, T. et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 385, 1975–1982 (2015).
Lunney, M. et al. Availability, accessibility, and quality of conservative kidney management worldwide. Clin. J. Am. Soc. Nephrol. 16, 79–87 (2021).
Kaur, G. et al. Cost of hemodialysis in a public sector tertiary hospital of India. Clin. Kidney J. 11, 726–733 (2018).
Ashuntantang, G. et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob. Health 5, e408–e417 (2017).
Olowu, W. A. et al. Outcomes of acute kidney injury in children and adults in sub-Saharan Africa: a systematic review. Lancet Glob. Health 4, e242–e250 (2016).
Jamison, D. T. et al. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd edn Vol. 9 (World Bank, 2017); https://doi.org/10.1596/978-1-4648-0527-1.
Teerawattananon, Y., Dabak, S. V., Khoe, L. C., Bayani, D. B. S. & Isaranuwatchai, W. To include or not include: renal dialysis policy in the era of universal health coverage. BMJ 368, m82 (2020).
Luyckx, V. A., Miljeteig, I., Ejigu, A. M. & Moosa, M. R. Ethical challenges in the provision of dialysis in resource-constrained environments. Semin. Nephrol. 37, 273–286 (2017).
Okpechi, I. G. et al. Building optimal and sustainable kidney care in low resource settings: the role of healthcare systems. Nephrology 26, 948–960 (2021).
Katz, I. J., Gerntholtz, T. & Naicker, S. Africa and nephrology: the forgotten continent. Nephron Clin. Pract. 117, 320–327 (2010).
Van Biesen, W. et al. Considerations on equity in management of end-stage kidney disease in low- and middle-income countries. Kidney Int. Suppl. 10, e63–e71 (2020).
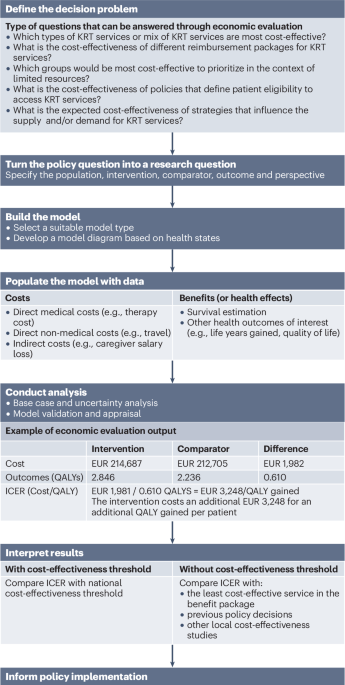
Drummond, M. F., Sculpher, M. J., Claxton, K., Stoddart, G. L., Torrance, G. W. Methods for the Economic Evaluation of Health Care Programmes. Oxford Univ. Press2015.
World Health Organization. 2015 Global Survey on Health Technology Assessment by National Authorities: Main Findings. https://iris.who.int/bitstream/handle/10665/375063/9789241509749-eng.pdf?sequence=1 (2015).
Kim, D. D. et al. Developing criteria for health economic quality evaluation tool. Value Health 26, 1225–1234 (2023).
Caro, J. J., Briggs, A. H., Siebert, U. & Kuntz, K. M. Modeling good research practices — overview: a report of the ISPOR-SMDM modeling good research practices task force-1. Value Health 15, 796–803 (2012).
Edwards, R. T. & McIntosh, E. (eds). Applied Health Economics for Public Health Practice and Research (Oxford Univ. Press, 2019); https://doi.org/10.1093/med/9780198737483.001.0001.
Meltzer, M. I. Introduction to health economics for physicians. Lancet 358, 993–998 (2001).
Roberts, M. et al. Conceptualizing a model: a report of the ISPOR-SMDM modeling good research practices task force-2. Value Health 15, 804–811 (2012).
Davies, M. & Cassimjee, Z. Provision of long-term renal replacement therapy to non-national patients in South Africa. South. Afr. Med. J. 111, 615 (2021).
Thaweethamcharoen, T., Sritippayawan, S., Noparatayaporn, P. & Aiyasanon, N. Cost-utility analysis of continuous ambulatory peritoneal dialysis and automated peritoneal dialysis for Thai patients with end-stage renal disease. Value Health Reg. Issues 21, 181–187 (2020).
Bayani, D. B. S. et al. Filtering for the best policy: an economic evaluation of policy options for kidney replacement coverage in the Philippines. Nephrology 26, 170–177 (2021).
Li, B. et al. Equity–efficiency trade-offs associated with alternative approaches to deceased donor kidney allocation: a patient-level simulation. Transplantation 104, 795–803 (2020).
Spinowitz, B. et al. Economic and quality of life burden of anemia on patients with CKD on dialysis: a systematic review. J. Med. Econ. 22, 593–604 (2019).
Gupta, D. et al. Peritoneal dialysis — first initiative in India: a cost-effectiveness analysis. Clin. Kidney J. 15, 128–135 (2022).
Erbe, A. W., Kendzia, D., Busink, E., Carroll, S. & Aas, E. Value of an integrated home dialysis model in the United Kingdom: a cost-effectiveness analysis. Value Health 26, 984–994 (2023).
Chalkidou, K., Culyer, A. J. & Nemzoff, C. Perspective in Economic Evaluations of Health Care Interventions in Low- and Middle-Income Countries — One Size Does Not Fit All. https://www.cgdev.org/sites/default/files/perspective-economic-evaluations-healthcare-interventions-low-and-middle-income.pdf (Center for Global Development, 2018).
Sittimart, M. et al. An overview of the perspectives used in health economic evaluations. Cost. Eff. Resour. Alloc.22, 41 (2024).
Drummond, M. et al. Transferability of economic evaluations across jurisdictions: ISPOR good research practices task force report. Value Health 12, 409–418 (2009).
Sassi, F. Calculating QALYs, comparing QALY and DALY calculations. Health Policy Plan. 21, 402–408 (2006).
Donnelly, J. Comparative effectiveness research (updated). Health Aff. (Millwood) https://doi.org/10.1377/hpb20101008.552571 (2010).
Rand, L. Z. & Kesselheim, A. S. Controversy over using quality-adjusted life-years in cost-effectiveness analyses: a systematic literature review. Health Aff. 40, 1402–1410 (2021).
Beresniak, A. et al. Validation of the underlying assumptions of the quality-adjusted life-years outcome: results from the ECHOUTCOME European project. Pharmacoeconomics 33, 61–69 (2015).
Anand, S. & Hanson, K. Disability-adjusted life years: a critical review. J. Health Econ. 16, 685–702 (1997).
Tomeny, E. M. et al. Rethinking tuberculosis morbidity quantification: a systematic review and critical appraisal of TB disability weights in cost-effectiveness analyses. Pharmacoeconomics 42, 1209–1236 (2024).
Arnesen, T. & Nord, E. The value of DALY life: problems with ethics and validity of disability adjusted life years. BMJ 319, 1423–1425 (1999).
Sanders, G. D. et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA 316, 1093–1103 (2016).
Sharma, D., Aggarwal, A. K., Downey, L. E. & Prinja, S. National healthcare economic evaluation guidelines: a cross-country comparison. Pharmacoecon. Open. 5, 349–364 (2021).
Daccache, C., Karam, R., Rizk, R., Evers, S. M. A. A. & Hiligsmann, M. The development process of economic evaluation guidelines in low- and middle-income countries: a systematic review. Int. J. Technol. Assess. Health Care 38, e35 (2022).
Verguet, S., Kim, J. J. & Jamison, D. T. Extended cost-effectiveness analysis for health policy assessment: a tutorial. Pharmacoeconomics 34, 913–923 (2016).
Norheim, O. F. et al. Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost. Eff. Resour. Alloc. 12, 18 (2014).
Elsayed, M. E., Morris, A. D., Li, X., Browne, L. D. & Stack, A. G. Propensity score matched mortality comparisons of peritoneal and in-centre haemodialysis: systematic review and meta-analysis. Nephrol. Dial. Transplant. 35, 2172–2182 (2020).
Luo, P.-T. et al. Impact of peritoneal dialysis modality on patient and PD survival: a systematic review. Perit. Dial. Int. 43, 128–138 (2023).
Chander, S. et al. Mortality and mode of dialysis: meta-analysis and systematic review. BMC Nephrol. 25, 1 (2024).
Cheng, L., Hu, N., Song, D. & Chen, Y. Mortality of peritoneal dialysis versus hemodialysis in older adults: an updated systematic review and meta-analysis. Gerontology 70, 461–478 (2024).
Zazzeroni, L., Pasquinelli, G., Nanni, E., Cremonini, V. & Rubbi, I. Comparison of quality of life in patients undergoing hemodialysis and peritoneal dialysis: a systematic review and meta-analysis. Kidney Blood Press. Res. 42, 717–727 (2017).
Chauhan, A. S. et al. Validating the rigour of adaptive methods of economic evaluation. BMJ Glob. Health 8, e012277 (2023).
Karopadi, A. N., Mason, G., Rettore, E. & Ronco, C. Cost of peritoneal dialysis and haemodialysis across the world. Nephrol. Dial. Transplant. 28, 2553–2569 (2013).
Ready, A. R., Nath, J., Milford, D. V., Adu, D. & Jewitt-Harris, J. Establishing sustainable kidney transplantation programs in developing world countries: a 10-year experience. Kidney Int. 90, 916–920 (2016).
Nemzoff, C. et al. Rapid cost-effectiveness analysis: hemodialysis versus peritoneal dialysis for patients with acute kidney injury in Rwanda. Cost. Eff. Resour. Alloc. 22, 35 (2024).
Wilkinson, T. et al. The international decision support initiative reference case for economic evaluation: an aid to thought. Value Health 19, 921–928 (2016).
Attema, A. E., Brouwer, W. B. F. & Claxton, K. Discounting in economic evaluations. Pharmacoeconomics 36, 745–758 (2018).
Haacker, M., Hallett, T. B. & Atun, R. On discount rates for economic evaluations in global health. Health Policy Plan. 35, 107–114 (2020).
Haacker, M., Hallett, T. B. & Atun, R. On time horizons in health economic evaluations. Health Policy Plan. 35, 1237–1243 (2020).
Adeagbo, C. U., Rattanavipapong, W., Guinness, L. & Teerawattananon, Y. The development of the guide to economic analysis and research (GEAR) online resource for low- and middle-income countries’ health economics practitioners: a commentary. Value Health 21, 569–572 (2018).
Bertram, M. Y., Lauer, J. A., Stenberg, K. & Edejer, T. T. T. Methods for the economic evaluation of health care interventions for priority setting in the health system: an update from WHO CHOICE. Int. J. Health Policy Manag. 10, 673–677 (2021).
Canadian Agency for Drugs and Technologies in Health. Guidelines for the Economic Evaluation of Health Technologies: Canada 4th edn. https://www.cda-amc.ca/sites/default/files/pdf/guidelines_for_the_economic_evaluation_of_health_technologies_canada_4th_ed.pdf (2017).
Harper, A., Mustafee, N. & Yearworth, M. Facets of trust in simulation studies. Eur. J. Oper. Res. 289, 197–213 (2021).
Stahl, J. E. Modelling methods for pharmacoeconomics and health technology assessment. Pharmacoeconomics 26, 131–148 (2008).
Siebert, U. et al. State-transition modeling. Med. Decis. Mak. 32, 690–700 (2012).
Soares, M. et al. Recommendations on the use of structured expert elicitation protocols for healthcare decision making: a good practices report of an ISPOR task force. Value Health 27, 1469–1478 (2024).
Goeree, R. et al. Transferability of economic evaluations: approaches and factors to consider when using results from one geographic area for another. Curr. Med. Res. Opin. 23, 671–682 (2007).
Teerawattananon, Y. & Tritasavit, N. A learning experience from price negotiations for vaccines. Vaccine 33, A11–A12 (2015).
Turner, H. C., Lauer, J. A., Tran, B. X., Teerawattananon, Y. & Jit, M. Adjusting for inflation and currency changes within health economic studies. Value Health 22, 1026–1032 (2019).
Vassall, A. et al. Reference Case for Estimating the Costs of Global Health Services and Interventions. https://ghcosting.org/pages/standards/reference_case (2017).
NICE Decision Support Unit. Survival Analysis TSD. https://www.sheffield.ac.uk/nice-dsu/tsds/survival-analysis (2022).
Coyle, D., Haines, A. & Lee, K. Extrapolating Clinical Evidence within Economic Evaluations: CADTH Methods and Guidelines (Canadian Agency for Drugs and Technologies in Health, 2023); https://www.ncbi.nlm.nih.gov/books/NBK594389/.
Afiatin et al. Economic evaluation of policy options for dialysis in end-stage renal disease patients under the universal health coverage in Indonesia. PLoS ONE12, e0177436 (2017).
Wyld, M., Morton, R. L., Hayen, A., Howard, K. & Webster, A. C. A systematic review and meta-analysis of utility-based quality of life in chronic kidney disease treatments. PLoS Med. 9, e1001307 (2012).
Liem, Y. S., Bosch, J. L. & Hunink, M. G. M. Preference-based quality of life of patients on renal replacement therapy: a systematic review and meta-analysis. Value Health 11, 733–741 (2008).
Chuasuwan, A., Pooripussarakul, S., Thakkinstian, A., Ingsathit, A. & Pattanaprateep, O. Comparisons of quality of life between patients underwent peritoneal dialysis and hemodialysis: a systematic review and meta-analysis. Health Qual. Life Outcomes 18, 191 (2020).
Jensen, C. E., Sørensen, P. & Petersen, K. D. In Denmark kidney transplantation is more cost-effective than dialysis. Dan. Med. J. 61, A4796 (2014).
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2021 (GBD 2021) Disability Weights (Institute for Health Metrics and Evaluation, 2024); https://doi.org/10.6069/485b-dx41.
Bilcke, J. & Beutels, P. Generating, presenting, and interpreting cost-effectiveness results in the context of uncertainty: a tutorial for deeper knowledge and better practice. Med. Decis. Mak. 42, 421–435 (2022).
Sullivan, S. D. et al. Budget impact analysis — principles of good practice: report of the ISPOR 2012 budget impact analysis good practice II task force. Value Health 17, 5–14 (2014).
Mauskopf, J. A. et al. Principles of good practice for budget impact analysis: report of the ISPOR task force on good research practices — budget impact analysis. Value Health 10, 336–347 (2007).
Briggs, A. H. et al. Model parameter estimation and uncertainty: a report of the ISPOR-SMDM modeling good research practices task force-6. Value Health 15, 835–842 (2012).
Chen, H.-F. et al. The magnitude of the health and economic impact of increased organ donation on patients with end-stage renal disease. MDM Policy Pract. 6, 23814683211063418 (2021).
Axelrod, D. A. et al. An economic assessment of contemporary kidney transplant practice. Am. J. Transplant. 18, 1168–1176 (2018).
NICE. in NICE Health Technology Evaluations: The Manual (National Institute for Health and Care Excellence, 2023).
Thokala, P., Ochalek, J., Leech, A. A. & Tong, T. Cost-effectiveness thresholds: the past, the present and the future. Pharmacoeconomics 36, 509–522 (2018).
Isaranuwatchai, W. et al. An empirical study looking at the potential impact of increasing cost-effectiveness threshold on reimbursement decisions in Thailand. Health Policy Technol. 13, 100927 (2024).
Bertram, M. Y. et al. Cost–effectiveness thresholds: pros and cons. Bull. World Health Organ. 94, 925 (2016).
Mangoya, D., Barham, L., Moyo, E., Moyo, P. & Dzinamarira, T. The use of economic evaluation tools in essential health benefits package selection for universal health coverage. Value Health Reg. Issues 36, 1–9 (2023).
Eregata, G. T. et al. Generalised cost-effectiveness analysis of 159 health interventions for the Ethiopian essential health service package. Cost. Eff. Resour. Alloc. 19, 2 (2021).
Eckman, M. H., Woodle, E. S., Thakar, C. V., Alloway, R. R. & Sherman, K. E. Cost-effectiveness of using kidneys from HCV-viremic donors for transplantation into HCV-uninfected recipients. Am. J. Kidney Dis. 75, 857–867 (2020).
Pichon-Riviere, A., Drummond, M., Palacios, A., Garcia-Marti, S. & Augustovski, F. Determining the efficiency path to universal health coverage: cost-effectiveness thresholds for 174 countries based on growth in life expectancy and health expenditures. Lancet Glob. Health 11, e833–e842 (2023).
Sampson, C. et al. Supply-side cost-effectiveness thresholds: questions for evidence-based policy. Appl. Health Econ. Health Policy 20, 651–667 (2022).
Strong, M., Oakley, J. E. & Chilcott, J. Managing structural uncertainty in health economic decision models: a discrepancy approach. J. R. Stat. Soc. Ser. C. Appl. Stat. 61, 25–45 (2012).
Haji Ali Afzali, H., Bojke, L. & Karnon, J. Model structuring for economic evaluations of new health technologies. Pharmacoeconomics 36, 1309–1319 (2018).
Jackson, C. H. et al. Value of information analysis in models to inform health policy. Annu. Rev. Stat. Appl. 9, 95 (2022).
Senanayake, S., Healy, H., McPhail, S. M., Baboolal, K. & Kularatna, S. Cost-effectiveness and budget impact analysis of implementing a ‘Soft Opt-Out’ system for kidney donation in Australia. Appl. Health Econ. Health Policy 20, 769–779 (2022).
Botwright, S., Win, E. M., Kapol, N., Benjawan, S. & Teerawattananon, Y. Cost-utility analysis of universal maternal pertussis immunisation in Thailand: a comparison of two model structures. Pharmacoeconomics 41, 77–91 (2023).
Rothery, C. et al. Value of information analytical methods: report 2 of the ISPOR value of information analysis emerging good practices task force. Value Health 23, 277–286 (2020).
Fenwick, E. et al. Value of information analysis for research decisions — an introduction: report 1 of the ISPOR value of information analysis emerging good practices task force. Value Health 23, 139–150 (2020).
Fenwick, E., Marshall, D. A., Levy, A. R. & Nichol, G. Using and interpreting cost-effectiveness acceptability curves: an example using data from a trial of management strategies for atrial fibrillation. BMC Health Serv. Res. 6, 52 (2006).
Jackson, C., et al. A guide to value of information methods for prioritising research in health impact modelling. Epidemiol. Methods 10, 20210012.
Health Intervention and Technology Assessment Program. Guidelines comparison. Guide to Economic Analysis and Research (GEAR) Online Resource. https://www.gear4health.com/gear/health-economic-evaluation-guidelines (2024).
Philips, Z., Bojke, L., Sculpher, M., Claxton, K. & Golder, S. Good practice guidelines for decision-analytic modelling in health technology assessment. Pharmacoeconomics 24, 355–371 (2006).
Husereau, D. et al. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Pharmacoeconomics 40, 601–609 (2022).
Eddy, D. M. et al. Model transparency and validation. Med. Decis. Mak. 32, 733–743 (2012).
World Health Organization. Value-based Pricing: WHO Guideline on Country Pharmaceutical Pricing Policies. A Plain Language Summary. https://iris.who.int/bitstream/handle/10665/341896/9789240024595-eng.pdf (2021).
Domínguez, J., Harrison, R. & Atal, R. Cost–benefit estimation of cadaveric kidney transplantation: the case of a developing country. Transpl. Proc. 43, 2300–2304 (2011).
Hryshchuk, S. M. & Parii, V. D. Cost-effectiveness of dialysis and kidney transplantation to treat end-stage renal disease in Ukraine. Wiad. Lekarskie 77, 765–771 (2024).
Rosselli, D., Rueda, J.-D. & Diaz, C. Cost-effectiveness of kidney transplantation compared with chronic dialysis in end-stage renal disease. Saudi J. Kidney Dis. Transplant. 26, 733 (2015).
Moradpour, A., Hadian, M. & Tavakkoli, M. Economic evaluation of end stage renal disease treatments in Iran. Clin. Epidemiol. Glob. Health 8, 199–204 (2020).
Hong, Z. et al. Economic evaluation of three dialysis methods in patients with end-stage renal disease in China. Int. Urol. Nephrol. 55, 1247–1254 (2022).
Pike, E., Hamidi, V., Ringerike, T., Wisloff, T. & Klemp, M. More use of peritoneal dialysis gives significant savings: a systematic review and health economic decision model. J. Clin. Med. Res. 9, 104–116 (2017).
Putri, S. et al. Supporting dialysis policy for end stage renal disease (ESRD) in Indonesia: an updated cost-effectiveness model. BMC Res. Notes 15, 359 (2022).
Sinclair, A. et al. Dialysis Modalities for the Treatment of End-Stage Kidney Disease: A Health Technology Assessment. CADTH Optimal Use Report No. 6.2b (Canadian Agency for Drugs and Technologies in Health, 2017); https://www.ncbi.nlm.nih.gov/books/NBK531991/.
Yang, F., Lau, T. & Luo, N. Cost-effectiveness of haemodialysis and peritoneal dialysis for patients with end-stage renal disease in Singapore. Nephrology 21, 669–677 (2016).
Liu, J. et al. Financial implications of dialysis modalities in the developing world: a Chinese perspective. Perit. Dial. Int. 40, 193–201 (2020).
Haller, M., Gutjahr, G., Kramar, R., Harnoncourt, F. & Oberbauer, R. Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol. Dial. Transplant. 26, 2988–2995 (2011).
Shimizu, U. et al. Cost-effectiveness achieved through changing the composition of renal replacement therapy in Japan. J. Med. Econ. 15, 444–453 (2012).
Surendra, N. K. et al. Cost utility analysis of end stage renal disease treatment in Ministry of Health dialysis centres, Malaysia: hemodialysis versus continuous ambulatory peritoneal dialysis. PLoS ONE14, e0218422 (2019).
Villa, G. et al. Cost-effectiveness analysis of the Spanish renal replacement therapy program. Perit. Dial. Int. 32, 192–199 (2012).
Treharne, C., Liu, F. X., Arici, M., Crowe, L. & Farooqui, U. Peritoneal dialysis and in-centre haemodialysis: a cost-utility analysis from a UK payer perspective. Appl. Health Econ. Health Policy 12, 409–420 (2014).
Yang, F., Liao, M., Wang, P. & Liu, Y. Cost-effectiveness analysis of renal replacement therapy strategies in Guangzhou city, southern China. BMJ Open. 11, e039653 (2021).
Yousefi, M., Rezaei, S., Hajebrahimi, S., Falsafi, N. & Keshvari-Shad, F. Peritoneal dialysis vs. hemodialysis among patients with end-stage renal disease in Iran: which is more cost-effective? BMC Nephrol. 25, 85 (2024).
Beby, A. T., Cornelis, T., Zinck, R. & Liu, F. X. Cost-effectiveness of high dose hemodialysis in comparison to conventional in-center hemodialysis in the Netherlands. Adv. Ther. 33, 2032–2048 (2016).
Liu, F. X., Treharne, C., Arici, M., Crowe, L. & Culleton, B. High-dose hemodialysis versus conventional in-center hemodialysis: a cost-utility analysis from a UK payer perspective. Value Health 18, 17–24 (2015).
Ramponi, F. et al. Cost-effectiveness analysis of online hemodiafiltration versus high-flux hemodialysis. Clinicoecon. Outcomes Res. 8, 531–540 (2016).
Augustyńska, J. et al. Automated peritoneal dialysis with remote patient monitoring: clinical effects and economic consequences for Poland. Value Health Reg. Issues 40, 53–62 (2024).
Moosa, M. R., Maree, J. D., Chirehwa, M. T. & Benatar, S. R. Use of the ‘Accountability for Reasonableness’ approach to improve fairness in accessing dialysis in a middle-income country. PLoS ONE11, e0164201 (2016).
Kiberd, B. A., Tennankore, K. K. & Vinson, A. J. Comparing the net benefits of adult deceased donor kidney transplantation for a patient on the preemptive waiting list vs a patient receiving dialysis. JAMA Netw. Open 5, e2223325 (2022).
Senanayake, S. et al. Deceased donor kidney allocation: an economic evaluation of contemporary longevity matching practices. BMC Health Serv. Res. 20, 931 (2020).
Smith, J. M. et al. Cost implications of new national allocation policy for deceased donor kidneys in the United States. Transplantation 100, 879–885 (2016).
Wong, C. K. H. et al. Lifetime cost-effectiveness analysis of first-line dialysis modalities for patients with end-stage renal disease under peritoneal dialysis first policy. BMC Nephrol. 21, 42 (2020).
Axelrod, D. A. et al. The clinical and economic benefit of CMV matching in kidney transplant: a decision analysis. Transplantation 106, 1227–1232 (2022).
Bamforth, R. J. et al. Expanding access to high KDPI kidney transplant for recipients aged 60 y and older: cost utility and survival. Transpl. Direct 10, e1629 (2024).
Ellison, T. A. et al. Evaluating cost-effectiveness in using high-kidney donor profile index organs. Transpl. Proc. 55, 2333–2344 (2023).
Hedley, J. A. et al. Cost-effectiveness of interventions to increase utilization of kidneys from deceased donors with primary brain malignancy in an Australian setting. Transpl. Direct 9, e1474 (2023).
Kadatz, M., Klarenbach, S., Gill, J. & Gill, J. S. Cost-effectiveness of using kidneys from hepatitis C nucleic acid test-positive donors for transplantation in hepatitis C-negative recipients. Am. J. Transplant. 18, 2457–2464 (2018).
Senanayake, S. et al. Donor kidney quality and transplant outcome: an economic evaluation of contemporary practice. Value Health 23, 1561–1569 (2020).
Shah, K. K. et al. Cost-effectiveness of kidney transplantation from donors at increased risk of blood-borne virus infection transmission. Transplantation 107, 2028–2042 (2023).
Koto, P. et al. An ex-ante cost-utility analysis of the deemed consent legislation compared to expressed consent for kidney transplantations in Nova Scotia. Cost. Eff. Resour. Alloc. 20, 55 (2022).
Cavallo, M. C. et al. Cost-effectiveness of kidney transplantation from DCD in Italy. Transpl. Proc. 46, 3289–3296 (2014).
Barnieh, L., Gill, J. S., Klarenbach, S. & Manns, B. J. The cost-effectiveness of using payment to increase living donor kidneys for transplantation. Clin. J. Am. Soc. Nephrol. 8, 2165–2173 (2013).
Karnon, J. et al. Modeling using discrete event simulation. Med. Decis. Mak. 32, 701–711 (2012).
Health Intervention and Technology Assessment Program. Plant-A-Tree — an open access decision tree builder. Guide to Economic Analysis and Research (GEAR) Online Resource. https://www.gear4health.com/page/i/plant-a-tree (2024).
Manns, B. J., Taub, K. J. & Donaldson, C. Economic evaluation and end-stage renal disease: from basics to bedside. Am. J. Kidney Dis. 36, 12–28 (2000).
Glossary: Health Economic Terms. https://yhec.co.uk/resources/glossary/ (York Health Economics Consortium, 2016).
Glossary of Terms for Health Economics and Systematic Review. https://methods.cochrane.org/economics/sites/methods.cochrane.org.economics/files/public/uploads/ccemg_website_glossary.pdf.
International Society of Nephrology. The ISN Framework for Developing Dialysis Programs in Low-Resource Settings. https://www.theisn.org/wp-content/uploads/2021/03/ISN-Framework-Dialysis-Report-HIRES.pdf (2021).
Bertram, M., Dhaene, G. & Tan-Torres Edejer, T. (eds). Institutionalizing Health Technology Assessment Mechanisms: A How to Guide. https://www.who.int/publications/i/item/9789240020665 (World Health Organization, 2021).