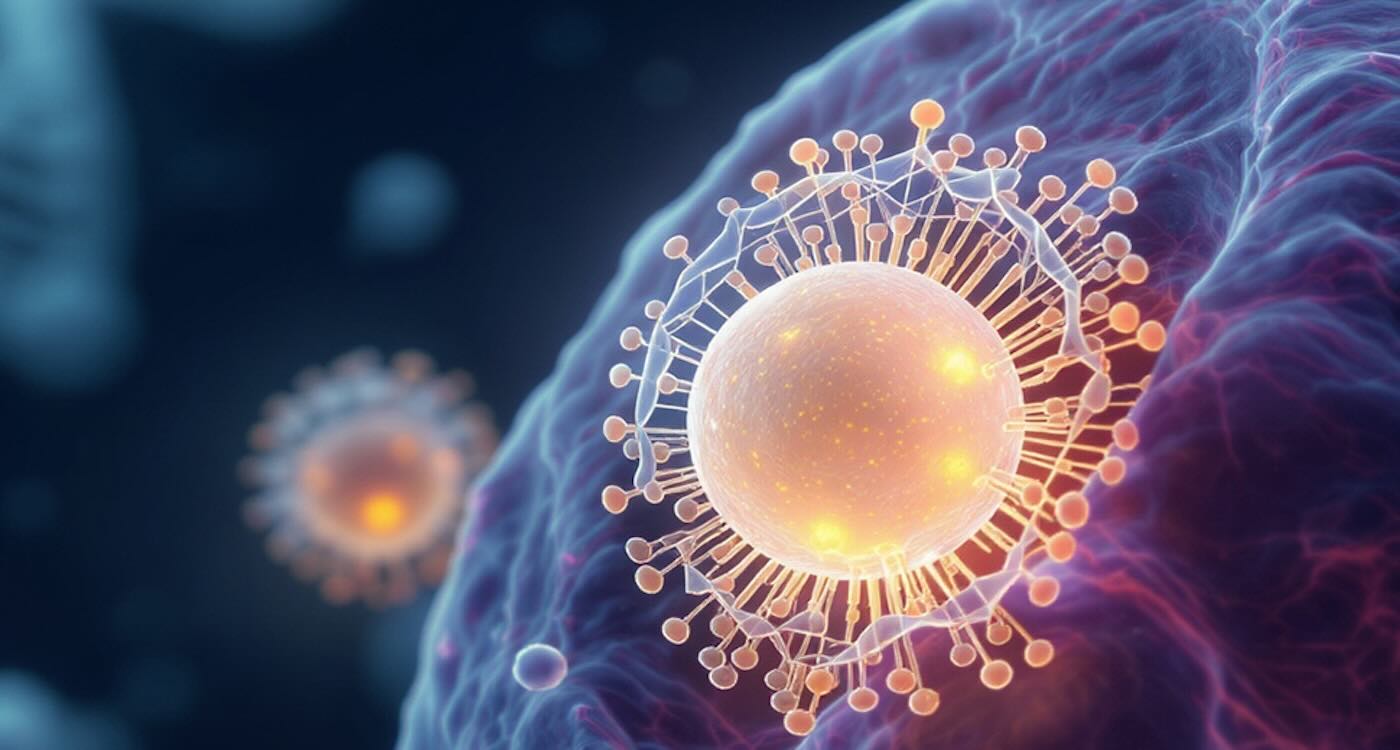
 Illustration of spherical nucleic acid SNA nanoparticle carrying CRISPR cargo – Image by the Mirkin Research Group
Illustration of spherical nucleic acid SNA nanoparticle carrying CRISPR cargo – Image by the Mirkin Research Group
University scientists in Chicago have developed a new nanostructure that triples CRISPR’s ability to enter cells, potentially unlocking even more power to treat genetic diseases.
With the power to rewrite the genetic code that underlies countless diseases, CRISPR holds immense promise to revolutionize medicine.
Now, Northwestern University chemists have unveiled a new type of nanostructure that dramatically improves CRISPR delivery and potentially extends its scope of utility.
CRISPR machinery cannot enter cells by itself. It always needs a delivery vehicle. Called ‘lipid nanoparticle spherical nucleic acids’ (LNP-SNAs), these tiny structures carry the full set of CRISPR editing tools—like Cas9 enzymes.
They’re wrapped in a dense, protective shell of DNA that dictates which organs and tissues the nanoparticles travel to and makes it easier for them to enter cells.
In lab tests across various human and animal cell types, the LNP-SNAs entered cells up to three times more effectively than the standard lipid particle delivery systems used for COVID-19 vaccines, caused far less toxicity and boosted gene-editing efficiency threefold.
The new nanostructures also improved the success rate of precise DNA repairs by more than 60% compared to current methods.
Their study, published in the Proceedings of the National Academy of Sciences, paves the way for safer, more reliable genetic medicines and underscores the importance of how a nanomaterial’s structure—rather than its ingredients alone—can determine its potency.
This principle underlies structural nanomedicine, an emerging field pioneered by Northwestern’s Chad A. Mirkin and his colleagues and pursued by hundreds of researchers around the world.
“CRISPR is an incredibly powerful tool that could correct defects in genes to decrease susceptibility to disease and even eliminate disease itself,” said Mirkin, who led the new study.
“But it’s difficult to get CRISPR into the cells and tissues that matter. Reaching and entering the right cells—and the right places within those cells—requires a minor miracle.
“We aimed to maximize CRISPR’s efficiency and expand the number of cell and tissue types that we can deliver it to.”
MORE GOOD CRISPR NEWS:
• Type 1 Diabetic Produces His Own Insulin After Gene-Edited Cell Transplant
• Aggressive Leukemia Disappears in 13-Year-old Girl Who was First to Receive New CRISPR Treatment
• Scientists Discover Potential HIV Cure that Eliminates Disease from Cells Using CRISPR-Cas Gene Editing
Scientists sometimes use viral vectors as the as a delivery vehicle. Naturally good at sneaking into cells, viruses are efficient, but they can cause the human body to mount an immune response, leading to painful or even dangerous side effects.
LNPs, on the other hand, are safer but inefficient. They tend to get stuck in endosomes, or compartments within the cell, where they cannot release their cargo.
“Only a fraction of the CRISPR machinery actually makes it into the cell and even a smaller fraction makes it all the way into the nucleus,” Mirkin said in a media release.
To overcome this barrier, Mirkin’s team turned to SNAs, which are globular — rather than linear — forms of DNA and RNA previously invented in Mirkin’s lab at Northwestern.
The spherical genetic material surrounds a nanoparticle core, which can be packed with cargo. Roughly 50 nanometers in diameter, the tiny structures possess a proven ability to enter cells for targeted delivery. Seven SNA-based therapies are already in human clinical trials, including a Phase 1b/2 clinical trial for solid tumors being developed by Flashpoint Therapeutics, a clinical-stage biotechnology startup.
In the new study, Mirkin’s team started with an LNP core carrying the CRISPR machinery inside. Then, they decorated the particle’s surface with a dense layer of short strands of DNA. Because the DNA can interact with a cell’s surface receptors, cells easily absorb SNAs. The DNA also can be engineered with sequences that target specific cell types, making delivery more selective.
MORE SUCCESS: CRISPR Identifies Commonly Available Drug That Works as Cobra Venom Antidote
“Simple changes to the particle’s structure can dramatically change how well a cell takes it up,” Mirkin said. “The SNA architecture is recognized by almost all cell types, so cells actively take up the SNAs and rapidly internalize them.”
Boosted performance across the board
After successfully synthesizing LNP-SNAs with CRISPR cargo, Mirkin and his team added them to cellular cultures, which included skin cells, white blood cells, human bone marrow stem cells, and human kidney cells.
Then, the team observed and measured several key factors: how efficiently the cells internalized the particles, whether the particles were toxic to cells and if the particles successfully delivered a gene. They also analyzed the cells’ DNA to determine if CRISPR had made the desired gene edits.
In every category, the system demonstrated its ability to successfully deliver CRISPR machinery and enable complex genetic modifications.
RELATED BREAKTHROUGH: 3 Years After CRISPR Treatment 73 of 75 Patients Cured of Blood Disease – FDA Approval is Near
Next, Mirkin plans to further validate the system in multiple in vivo disease models. The university’s biotechnology spin-out Flashpoint Therapeutics is commercializing the technology with the goal of rapidly moving it toward clinical trials.
“CRISPR could change the whole field of medicine,” Mirkin said. “But how we design the delivery vehicle is just as important as the genetic tools themselves.
“By marrying two powerful biotechnologies — CRISPR and SNAs — we have created a strategy that could unlock CRISPR’s full therapeutic potential.”
SHARE THE CRISPR NEWS With Science Geeks on Social Media…
