The 50th Annual Society for Pediatric Dermatology (SPD) Meeting brought together clinicians, researchers, and trainees from across the globe to discuss the latest advances in pediatric skin care. Known for its collaborative atmosphere and focus on clinical practice and research, the SPD conference continues to serve as a central forum for exchanging ideas in this rapidly evolving specialty. This year’s meeting featured a broad spectrum of sessions, from therapeutic innovations to rare disease management, with particular attention given to emerging diagnostic tools such as molecular and genetic testing. Among the expert voices was Virginia Sybert, MD, a renowned pediatric dermatologist and medical geneticist, who shared her perspective with Dermatology Times on the thoughtful use of DNA testing in dermatology practice.
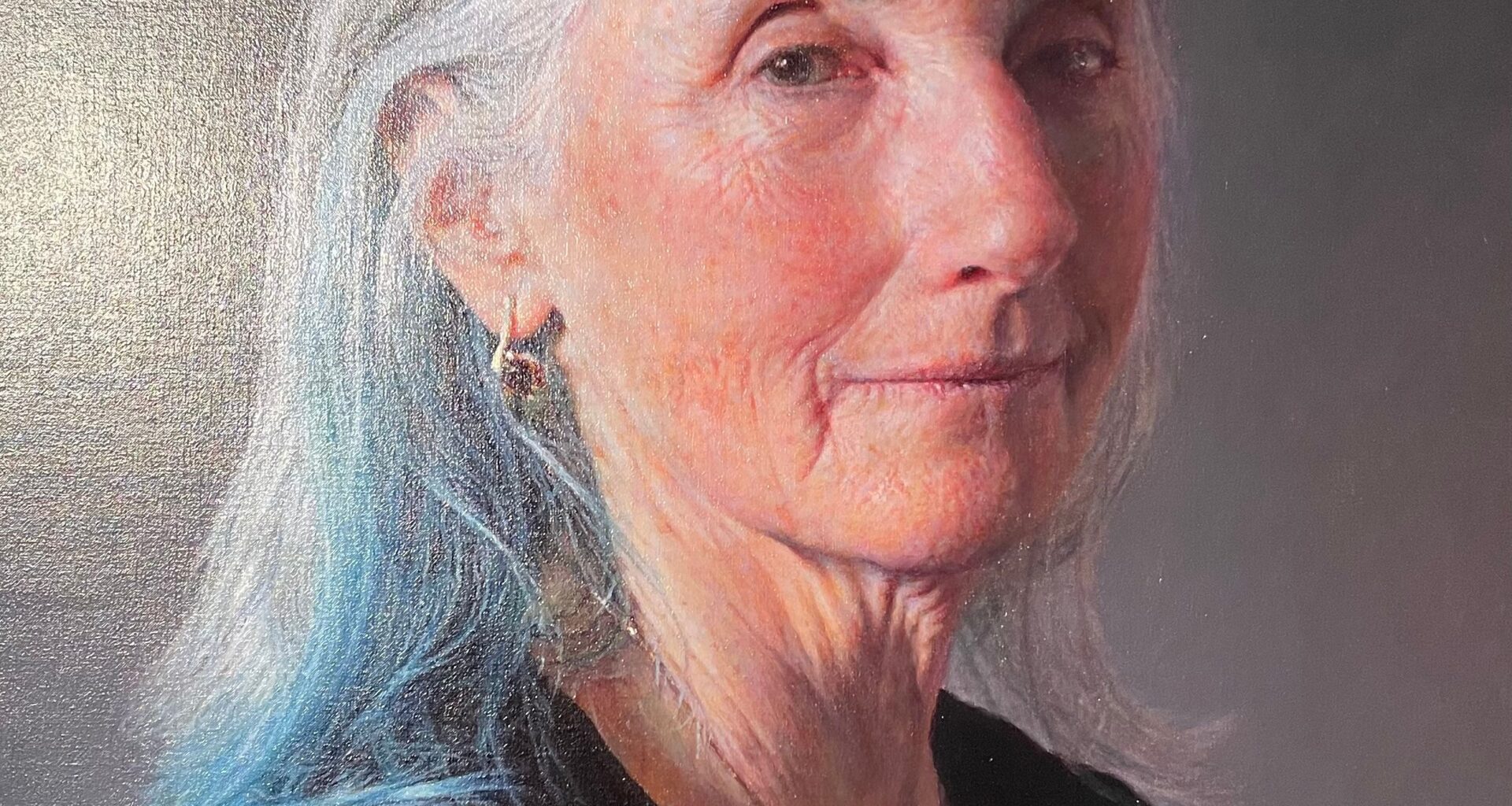
Sybert, who recently retired from clinical care after decades at Seattle Children’s Hospital and the University of Washington as well as stints at Group Health and Kaiser, brings a unique dual background in dermatology and medical genetics. Her session focused on the role of molecular diagnostics in identifying and managing inherited dermatologic conditions—a topic that bridges 2 highly specialized fields.
According to Sybert, the integration of genetic testing into dermatologic care rests on 3 critical principles: ensuring the necessity of the test, selecting the appropriate type of testing, and having the expertise to interpret results accurately. “Number 1, you want to make sure that you’re doing testing that’s necessary,” she explained. “Number 2, that you’re doing the right kind of testing, and number 3, that you know how to interpret those results.”
She emphasized that these steps can present challenges in day-to-day clinical practice. For this reason, she advocates for close collaboration between clinicians, leveraging each specialty’s strengths to optimize patient outcomes. “I really encourage the interaction of geneticists and dermatologists to deal with all of these things,” she noted.
While acknowledging that genetic testing remains underutilized in diagnosing many inherited dermatologic conditions, Sybert expressed equal concern about inappropriate overuse. Ordering tests without a clear clinical indication or without the expertise to interpret complex genetic data, she cautioned, can create confusion, unnecessary expense, and potential harm. “I am a little bit more concerned when it’s overutilized, when it is used when it is not appropriate,” she said.
Historically, cost has been a barrier to the widespread adoption of molecular diagnostics. However, Sybert pointed out that genetic testing is now comparatively less expensive than many other forms of medical care. Despite this, hesitancy persists among clinicians and patients, partly due to the complexity of result interpretation and lingering uncertainty about the implications of genetic findings.
The difficulty lies not just in identifying pathogenic variants, but also in determining their relevance to a patient’s phenotype and prognosis. Many results fall into the category of “variants of uncertain significance,” which require careful correlation with clinical findings and, often, additional family studies. This complexity underscores her call for multidisciplinary involvement and specialized knowledge in genetic evaluation.
Sybert’s insights align with a broader trend in medicine toward precision care—tailoring diagnosis and management strategies to the unique genetic makeup of individual patients. In dermatology, this can have particularly high impact in the context of rare genodermatoses, where early and accurate diagnosis may influence surveillance strategies, treatment decisions, and family counseling.
The SPD meeting, she reflected, represents an environment where such multidisciplinary dialogue thrives. From its beginnings as a small, tight-knit group, the organization has grown significantly while maintaining its inclusive and supportive culture. “People are very nice, and they’re very inclusive, and we think we’re very supportive of younger people,” she said, crediting the late Nancy B. Esterly, MD, as one of the society’s touchstones. This sense of community is especially valuable in advancing fields like genetic dermatology, which require shared expertise across specialties.
For clinicians in pediatric dermatology, Sybert’s take-home message was clear: Genetic testing is a powerful tool when used judiciously and in the right clinical context. The future of dermatologic care, she suggested, will increasingly rely on harnessing molecular data—not in isolation, but as part of a comprehensive, patient-centered approach.
As the specialty moves forward, sessions like Sybert’s at SPD 2025 highlight both the opportunities and responsibilities that come with cutting-edge diagnostics. Careful stewardship of these tools, coupled with collaboration and ongoing education, will be key in realizing their full potential for improving pediatric skin health.