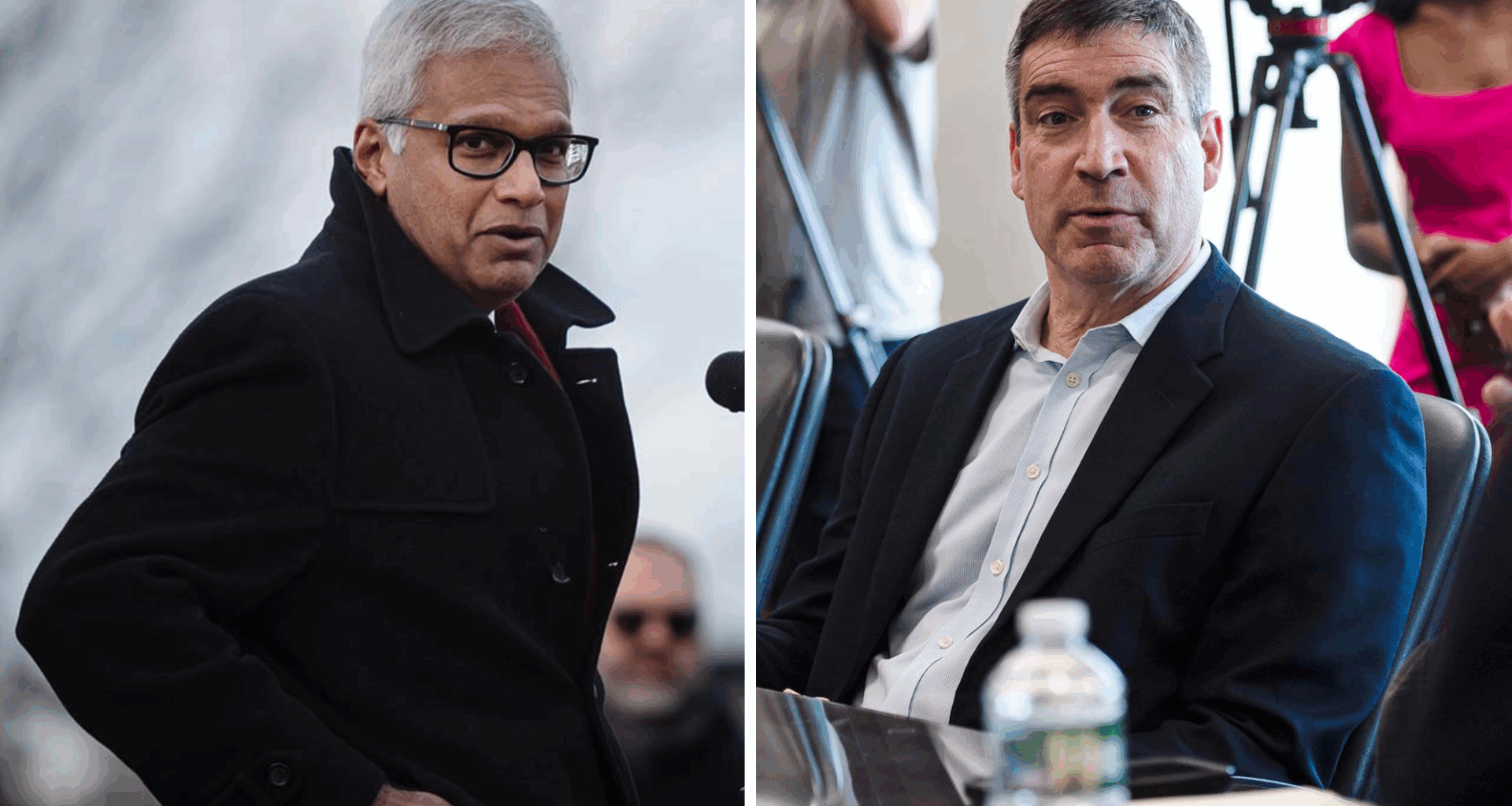
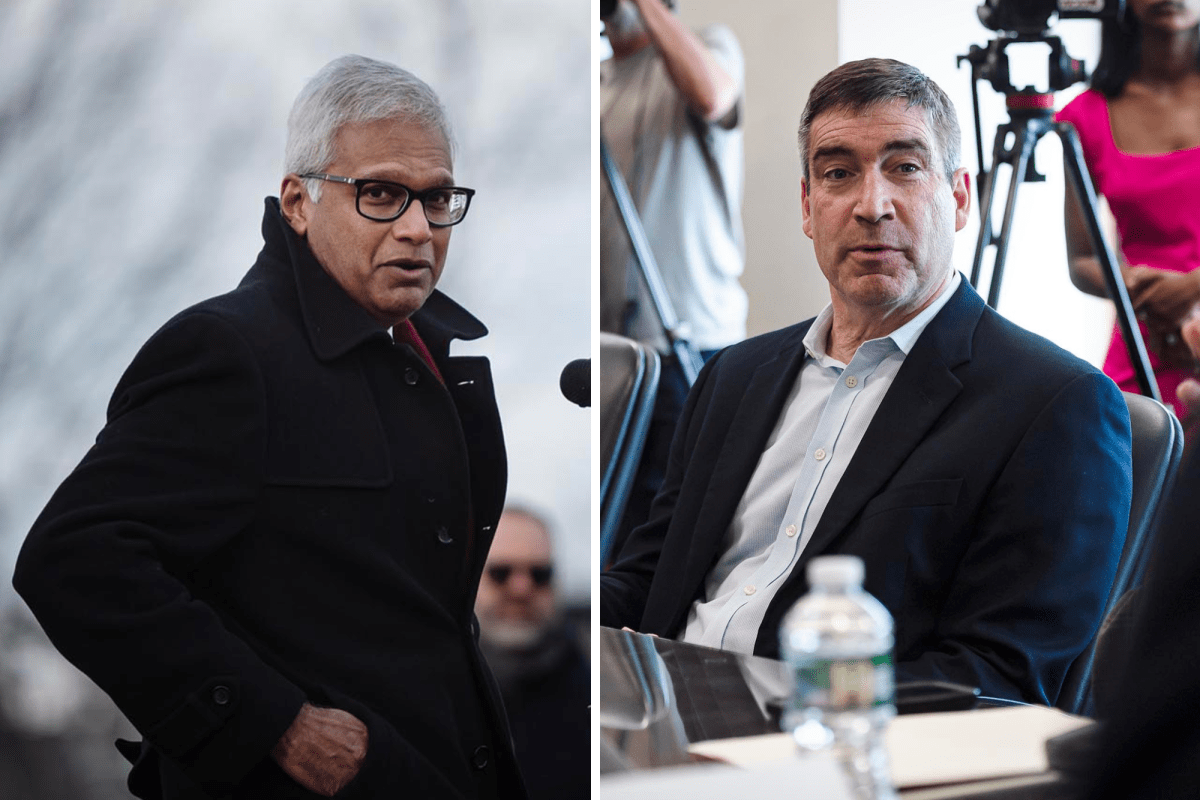
 Sunny Eappen and Stephen Leffler. Photos by Glenn Russell/VTDigger
Sunny Eappen and Stephen Leffler. Photos by Glenn Russell/VTDigger
Steve Leffler, the president of UVM Medical Center, officially took the reins Wednesday as the new head of the rebranded UVM Health network. The new leadership signals a new vision for the hospital network, he and its board leadership say — one that emphasizes the hospitals’ work over the network’s.
Sunny Eappen’s resignation as the president and CEO at the network came the same week in mid-September that the state’s main health care regulator, the Green Mountain Care Board, set restrictive budget conditions on UVM Medical Center and its sibling hospitals. Still, Tom Golonka, chair of the network’s board of trustees, said he was surprised by Eappen’s decision to leave.
As he was getting ready for a joint board meeting to discuss the issues that the care board raised during hearings about the network hospitals’ budgets, Golonka received a call from Eappen informing him of his decision, he said.
READ MORE
by Olivia Gieger
September 15, 2025, 5:55 pmSeptember 16, 2025, 12:19 pm
“The board didn’t have a chance to talk about it, we had a meeting scheduled the next week,” Golonka said. “This wasn’t any type of force. We were completely prepared to support him for a period.”
At the Sept. 12 meeting of the Green Mountain Care Board, chair Owen Foster laid into the network, which includes the UVM Medical Center in Burlington, Central Vermont Medical Center in Berlin, Porter Medical Center in Middlebury, three hospitals in eastern New York state, and a home health and hospice care provider. Foster outlined what he called a “corporate shell game” of funds moving from the Medical Center’s reserves to the network and its New York hospitals.
The regulator’s chair also raised concerns about the high executive compensation and the widening gap between what the network’s leadership made each year and what its lowest paid employees earned — in 2024, 19 executives brought home a collective $3 million in bonuses alone.
Foster called the network both “physically and spiritually distant” from the needs of Vermonters and of the UVM Medical Center.
“That was hard to hear,” Leffler told VTDigger in an Oct. 10 interview. “It became clear that the vision needed to evolve and change a little bit.”
Eappen took that message to heart, both Leffler and Golonka said.
“After some really thoughtful reflection with the network board, [he] agreed that it’d be better to take a shift and for him to step away,” Leffler said.
Sunny believed that his stepping down was the best thing for him to do for the sake of the organization, Golonka said. “I really applaud him for his leadership,” he added. “It takes a really strong leader to be able to say that, and to envision a future that doesn’t include him.”
Course correction
The future that Leffler foresees will be network-lite, with more emphasis on allowing for the autonomy of its hospitals.
“It’s not going to be top down from the network. The network’s kind of in the background,” he said. “It’s not the center of the solar system. It’s kind of on the outer fringes,” Leffler explained.
“Now we are going to do a bit of course correction,” he added. “It’s a subtle shift, but it’s a giant shift at the same time.”
Already, the network has rebranded, with a new website and logos reading University of Vermont Health, dropping “network” from its name.
The new name echoes the labels used by Dartmouth Health — a network of six hospitals across New Hampshire and southern Vermont that includes a large academic medical center. It’s a model with more hospital autonomy that Leffler said he is looking to mirror. He described a structure where hospitals and staff on the floor lead decisions and drive change by working primarily with their own boards.
“I’m a big believer in [saying] the people close to the care know what’s best and know what needs to be done,” Leffler said. “If the network board is going to hear about six different hospitals, then how much time can you spend on any one issue?”
Previously, though, the network had answered that question by taking a heavier hand in management and governance, in the name of efficiency.
Originally, each hospital board hired and fired its own presidents, and they approved their own budgets that then the network staff and board would review and approve, explained UVM Medical Center Board Chair Jesse Bridges.
But as the network started to consolidate systems like their electronic medical records and human resources around 2022, the process quickly grew laborious and long. “It was process for the sake of process,” Bridges said.
Those adjustments resulted in the current streamlined system, where the network board makes the final fiduciary decisions, with input and recommendations from the partner boards.
“Before, there wasn’t coordination or control,” Golonka, the network board chair, described. “We were not rowing in the same direction.”
The challenge now is figuring out a governance structure that keeps all the boats moving in the same direction, while also letting each row on its own. To find that, “everything can be on the table,” Golonka said.
Though the rhetoric and governance around the network may be changing, it’s clear that the network structure of the hospital group is not. Leffler and both board chairs voiced a strong belief in the efficiencies that can come from the larger structure, for things like buying materials in bulk or streamlining HR processes and medical records.
Increasing quality
At the top of Leffler’s to-do list in the new role will be improving quality of care.
The Centers for Medicare & Medicaid Services assigns hospitals quality ratings, and the network hospitals’ numbers have dropped since 2022. Leffler is set on earning back UVM’s stars.
“At the very first meeting, we’re getting every quality scorecard from 2025 that we have, and we’re going to go over them. We’re going to make a commitment, all of us, every hospital, every clinic, every office, how we’re going to improve them over (20)26,” he said.
To do so, he wants those on the floor to lead the way, rather than having the network institute top-down changes.
Improvements to safety for patients and staff, increased access for rural patients, and improved affordability all fall on Leffler’s wishlist of what to address in his new role, he said. UVM Medical Center, where Leffler will remain in charge, is set to continue to play a key role.
“If we’re not playing the right role in all of those areas (of affordability and access), because we’re the biggest, everyone is going to be pointing at us saying, ‘You’re not doing your part,’ ” said Bridges, the medical center’s board chair.
Bridges cited the network’s recent partnership with Dartmouth Health on kidney transplant surgery. After UVM Medical Center averaged about 12 surgeries a year, it simply wasn’t cost effective to continue offering that care, as a state-commissioned consultant’s report on health care costs found. The partnership with Dartmouth allows patients to do pre- and post- surgery care in Burlington despite having surgery in the New Hampshire hospital.
“Access might have to look different in order to get at affordability and quality,” Bridges said, adding that it will require the network to look within its own system while also thinking on broader scales of partnerships at the state and regional levels.
Born and raised
Eappen joined the network in 2022 as it was still navigating the fallout of the Covid-19 pandemic. He came to Vermont after working as an administrator for 14 years at Brigham & Women’s Hospital in Boston. Under his leadership, the network saw more integration of processes and began to operate as an interlocking system, rather than a collection of affiliated hospitals, Leffler and Golonka both echoed.
Eappen took over after John Brumstead had led the hospital system for over a decade. Brumstead created the network, overseeing the initial effort to join UVM Medical Center with Central Vermont Medical Center, in 2011. The partnership grew to encompass six hospitals in the ensuing six years, taking the name University of Vermont Health Network in 2014.
“At the time Sunny was just the right guy to transition from John Brumstead, who was this kind of Vermont icon,” said Betsy Vicencio, the network board’s vice chair.
“Sunny just had a different way of trying to invite change and trying to invite new relationships. Clearly some were really successful and some that were maybe less than successful,” she said. “Vermont and New York, we don’t necessarily do different as well as other places. We have some cultural limits that are hard.”
Though Vicencio said she does not think Eappen himself focused or worried about being from outside Vermont, she does suspect that his Boston background contributed to some of the external pressures that ultimately led to his departure.
“It is absolutely within the cultural ethos of upstate New York and Vermont to not be as welcoming to people that are not born and raised here,” she said.
With Leffler, the network is returning to homegrown leadership.
He grew up in Leicester, Vt., where his parents owned a general store, he said. He completed medical school at the University of Vermont, before returning to the emergency department as a young doctor in 1993. He led the emergency department from 2006 to 2011, worked as the hospital’s chief medical officer, and then became the president of the medical center in 2020.
“I really care about this region. I care about the medical center. It’s my home. I care about the care that we deliver to my friends, my family, my kids and my grandkids,” Leffler said.
“Steve is Vermont’s beloved son, and he is Vermont’s beloved emergency room doc,” Vicencio said. “He is rural health care at its finest. He lives and breathes and has grown up in all of the things that are foundational to rural health care.”
She recalled first meeting Leffler at a trustee event when he first stepped into a leadership role nearly 10 years ago. She began asking him about how the hospital could possibly bring down health care costs and watched Leffler light up with ideas: “He was super energized, and he had a vision back then.”
“I think that he’s going to come in with this kind of refreshed view of making those particular pieces not just rhetoric, but real,” Vicencio said.
Bridges, of the medical center board, echoed that: “Even though [Leffler] has been here, it’s not going to be more of the same. It’s actually, I think, a fairly substantial change on the horizon.”
As part of his board chair role, Bridges does rounds through the hospital with Leffler every month. Through that, he’s come to know Leffler as an “honest broker” and eager listener, he said, having watched Leffler pay considerate attention to any patient or provider who approached him.
“I think part of what makes Steve successful is his willingness to listen, be humble, admit maybe when he said something has come out the wrong way,” Bridges said.