Hawaii’s two largest health care organizations on Wednesday unveiled a proposal to create what they describe as a more coordinated, affordable and accessible health care system — while stressing that the plan is not a merger, but rather a partnership that would keep existing hospitals and insurance operations intact.
Hawaii Medical Service Association and Hawai‘i Pacific Health said the proposal would bring the two local, nonprofit organizations under a new parent entity, tentatively called One Health Hawaii, while allowing each to continue operating independently as legal affiliates.
“It’s two local companies coming together under a new parent that will largely continue to operate each respectively the way they do with everybody else in the community on a going-forward basis,” Ray Vara, president and CEO of Hawai‘i Pacific Health, said during a Wednesday briefing.
The proposal comes as Hawaii faces rising health care costs, workforce shortages and concerns about long-term sustainability of the state’s medical system. HMSA insures more than 750,000 people statewide, while HPH operates major hospitals including Kapi‘olani Medical Center for Women &Children, Pali Momi Medical Center, Straub Medical Center and Wilcox Medical Center on Kauai.
Both organizations emphasized that the proposed affiliation would operate as an open system, unlike Kaiser Permanente’s closed model in which members typically receive care only within Kaiser facilities.
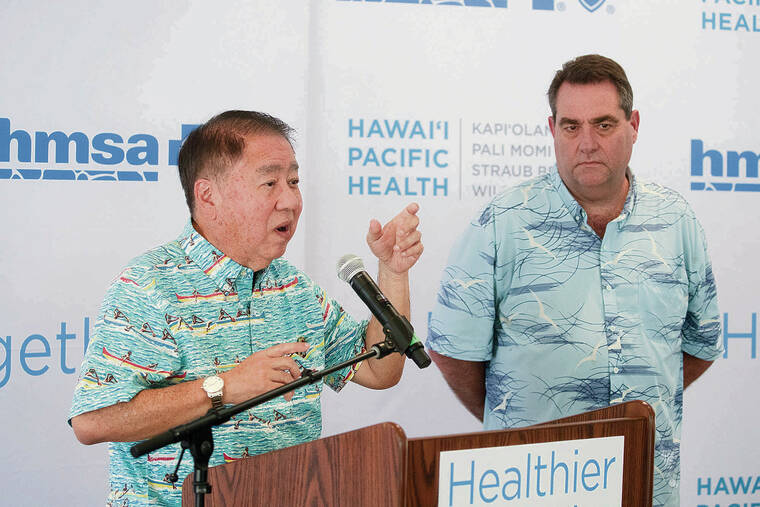
“This proposed system is an open system. Every provider will join. In fact, we need them to join,” HMSA CEO Mark Mugiishi said.
Don’t miss out on what’s happening!
Stay in touch with breaking news, as it happens, conveniently in your email inbox. It’s FREE!
Mugiishi said patients would retain the ability to choose their doctors and facilities, including providers not affiliated with HPH.
“We want our members to be able to see the doctor of their choice, to go to the facility of their choice,” he said.
He added that HMSA’s current spending is already broadly distributed across providers statewide.
“At HMSA, we pay one-third of our dollars to Queen’s, one-third of our dollars to independent providers, and one-third of our dollars to Hawai‘i Pacific Health,” Mugiishi said. “There is no universe in the world where we can say, ‘Well, we’ll just take two-thirds of them and not have them anymore.’ We need all of them.”
Vara said the proposal grew out of deep concern about Hawaii’s cost of living and the role health care plays in overall affordability.
“This is an exciting day, but it really comes from the premise of something that we all know all too well, and that is that we’ve got a real affordability issue here in the state of Hawaii,” Vara said. “Frankly, I would argue that it’s the greatest challenge facing our state.”
He tied rising costs to outmigration, particularly among young families.
“We’ve got thousands and thousands of people, year over year, that leave the state because they no longer can afford to live here,” he said. “We certainly know that for our young people, it’s nearly impossible to ask them to come home and return to this place that we love so much.”
He said health care costs are among the top contributors to affordability challenges statewide and warned about long-term sustainability.
“And as someone who’s an insider in the industry … I’m worried about its long-term sustainability,” Vara said.
Vara cited a personal experience involving his daughter to highlight what he described as failures in care coordination. He said his family faced weeks-long delays obtaining a necessary medical device after a physician ordered it, creating a risk of serious infection. The holdup, he said, ultimately came down to cost — a relatively inexpensive item that could have prevented a potentially costly and dangerous hospitalization.
“Now, here’s the irony of that situation,” he said. “That child was my daughter. And I am as close to the health care system as you can get. And we fell victim to it.”
He added, “We didn’t know what was going on, and it put our daughter at risk,” saying that eliminating such failures in coordination is central to the proposed system.
“If we can create a system that begins to eliminate that kind of risk and families to go through that, I promise you it’s work worth doing.”
Under the proposal, HMSA and HPH would become affiliates of One Health Hawaii, a new nonprofit parent organization. Vara said the plan would require extensive regulatory review.
“It’s going to have to go through a number of state agencies to include a certificate of need process,” he said, as well as review by the state attorney general, insurance commissioner and federal regulators.
“And then there’s also a federal approval that’s going to be required,” Vara said. “On the short side, it could be six months. On the long side, it could be 18 months or longer.”
Mugiishi said the organization’s mission — dating back 87 years — has always been to improve the health of Hawaii residents, but acknowledged growing challenges.
He said that access to care has become increasingly difficult in Hawaii, with patients facing long waits to see both primary care physicians and specialists, followed by high out-of-pocket costs; the proposed affiliation is meant to modernize health care delivery.
“It is time for structural change,” he said, comparing the health care system to companies that failed to evolve. “There’s a whole bunch of big, big companies in Hawaii that don’t exist today because they didn’t evolve.”
He said an integrated structure could support a shift away from fee-for-service medicine toward value-based care.
“We have a requirement that it has to be based on value, not just fee for service,” Mugiishi said. “We want it to be outcome based, like you generate value for this patient, for health care, then you will get paid.”
He reiterated that HMSA and HPH would remain separate entities, and not a merger.
“It’s because there’s a parent company that’s deciding strategy,” Mugiishi said. “HMSA will continue to operate as a legal affiliate of that parent. HPH will continue to operate as a legal affiliate.”
The announcement drew immediate criticism from The Queen’s Health Systems, Hawaii’s largest health care provider by market share.
“Queen’s has been opposed to the merger. We’ve been the most vocal in opposition over the past nine months,” said Jason Chang, president and CEO of The Queen’s Health Systems.
Chang said Queen’s believes the proposal could create an anti-competitive environment, even if described as an open network.
“We believe that it creates an environment that’s anti-competitive and will steer patients away from other health systems towards this new entity,” Chang said.
Chang warned that despite being described as open, a preferred network could steer patients by imposing higher costs or limiting access to doctors who are not included.
Queen’s relies on commercially insured patients to fund critical services such as trauma care, behavioral health and transplants.
“We’ve quantified that if 5% of our commercial business were to shift, it’s approximately $50 million of impact,” he said.
He warned that revenue losses could force difficult decisions.
“We’ve watched other hospitals in the state have to shut down programs,” Chang said. “Those are hard decisions to make, and we don’t want to get to a place, so we have to make those kinds of decisions.”
The Hawaii Nurses’ Association, which represents about 4,000 health care workers statewide, said it is seeking clarity on how the proposal would affect workers and patients.
“We wanted to make sure that we had our voice out there as well,” said Rosalee Agas-Yuu, the union’s president.
She said nurses across multiple systems have been raising questions.
“Our members include not only HPH members. You know, we have members in Queen’s. We have members that you know are on the outer islands,” Agas-Yuu said.
She emphasized the need for public engagement.
“As a community, we should all become informed,” she said. “We want to make sure that what’s going to be introduced is going to be beneficial for our community.”
Agas-Yuu said the union wants town halls and public forums to allow residents and workers to ask questions, and for nurses to be part of that conversation.
She also raised concerns about labor contracts and health insurance for workers, pointing to a string of recent nurses’ strikes across Hawaii tied to staffing shortages, wages and benefits.
“We fought hard for our contracts,” Agas-Yuu said. “So what are those contracts going to be?”
HMSA and HPH leaders said the proposal remains subject to regulatory approval and public scrutiny, with no immediate changes to coverage or hospital operations.
Supporters say the affiliation could help stabilize Hawaii’s health care system amid rising costs, while critics warn it could concentrate power and undermine competition.
As regulatory review moves forward, state officials, providers, unions and patients are expected to closely watch how the proposal unfolds — and whether it delivers on promises of affordability without limiting choice.