American Psychiatric Association. Diagnostic and statistical manual of mental disorders, Fifth Edition. Arlington, VA: American Psychiatric Publishing, Inc; 2013.
Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. J Psychiatr Res. 2018;104:235–48.
Pawluski JL, Lonstein JS, Fleming AS. The neurobiology of postpartum anxiety and depression. Trends Neurosci. 2017;40:106–20.
Al-abri K, Edge D, Armitage CJ. Prevalence and correlates of perinatal depression. Soc Psychiatry Psychiatr Epidemiol. 2023;58:1581–90.
Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3:973–82.
Hahn-Holbrook J, Cornwell-Hinrichs T, Anaya I. Economic and health predictors of national postpartum depression prevalence: a systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Front Psychiatry. 2018;8:248. https://doi.org/10.3389/fpsyt.2017.00248.
Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86–92.
Slomian J, Honvo G, Emonts P, Reginster JY, Bruyère O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health. 2019;15:1745506519844044.
Duan C, Cosgrove J, Deligiannidis KM. Understanding peripartum depression through neuroimaging: a review of structural and functional connectivity and molecular imaging research. Curr Psychiatry Rep. 2017;19:70.
Moses-Kolko EL, Horner MS, Phillips ML, Hipwell AE, Swain JE. In search of neural endophenotypes of postpartum psychopathology and disrupted maternal caregiving. J Neuroendocrinol. 2014;26:665–84.
Barba-Müller E, Craddock S, Carmona S, Hoekzema E. Brain plasticity in pregnancy and the postpartum period: links to maternal caregiving and mental health. Arch Womens Ment Health. 2019;22:289–99.
Orchard ER, Rutherford HJV, Holmes AJ, Jamadar SD. Matrescence: lifetime impact of motherhood on cognition and the brain. Trends Cogn Sci. 2023;27:302–16.
Cárdenas EF, Kujawa A, Humphreys KL. Neurobiological changes during the peripartum period: implications for health and behavior. Soc Cogn Affect Neurosci. 2019;15:1097–110.
Servin-Barthet C, Martínez-García M, Pretus C, Paternina-Die M, Soler A, Khymenets O, et al. The transition to motherhood: linking hormones, brain and behaviour. Nat Rev Neurosci. 2023;24:605–19.
Horáková A, Němcová H, Mohr P, Sebela A. Structural, functional, and metabolic signatures of postpartum depression: a systematic review. Front Psychiatry. 2022;13:1044995.
Stickel S, Wagels L, Wudarczyk O, Jaffee S, Habel U, Schneider F, et al. Neural correlates of depression in women across the reproductive lifespan – an fMRI review. J Affect Disord. 2019;246:556–70.
Radoš SN, Akik BK, Žutić M, Rodriguez-Muñoz MF, Uriko K, Motrico E, et al. Diagnosis of peripartum depression disorder: a state-of-the-art approach from the COST Action Riseup-PPD. Compr Psychiatry. 2024;130:152456.
Bernstein IH, Rush AJ, Yonkers K, Carmody TJ, Woo A, McConnell K, et al. Symptom features of postpartum depression: are they distinct? Depress Anxiety. 2008;25:20–6.
Luo F, Zhu Z, Du Y, Chen L, Cheng Y. Risk factors for postpartum depression based on genetic and epigenetic interactions. Mol Neurobiol. 2023;60:3979–4003.
Batt MM, Duffy KA, Novick AM, Metcalf CA, Epperson CN. Is postpartum depression different from depression occurring outside of the perinatal period? A review of the evidence. Focus J Life Long Learn Psychiatry. 2020;18:106.
Silverman ME, Loudon H, Safier M, Protopopescu X, Leiter G, Liu X, et al. Neural dysfunction in postpartum depression: an fMRI Pilot study. CNS Spectr. 2007;12:853–62.
Northoff G, Wiebking C, Feinberg T, Panksepp J. The ‘resting-state hypothesis’ of major depressive disorder—A translational subcortical–cortical framework for a system disorder. Neurosci Biobehav Rev. 2011;35:1929–45.
Nguyen AJ, Hoyer E, Rajhans P, Strathearn L, Kim S. A tumultuous transition to motherhood: altered brain and hormonal responses in mothers with postpartum depression. J Neuroendocrinol. 2019;31:e12794.
Payne JL, Maguire J. Pathophysiological mechanisms implicated in postpartum depression. Front Neuroendocrinol. 2019;52:165–80.
Goldstein-Piekarski AN, Ball TM, Samara Z, Staveland BR, Keller AS, Fleming SL, et al. Mapping neural circuit biotypes to symptoms and behavioral dimensions of depression and anxiety. Biological Psychiatry. 2022;91:561–71.
Cash RFH, Weigand A, Zalesky A, Siddiqi SH, Downar J, Fitzgerald PB, et al. Using brain imaging to improve spatial targeting of transcranial magnetic stimulation for depression. Biol Psychiatry. 2021;90:689–700.
Fox MD, Liu H, Pascual-Leone A. Identification of reproducible individualized targets for treatment of depression with TMS based on intrinsic connectivity. Neuroimage. 2013;66:151–60. https://doi.org/10.1016/j.neuroimage.2012.10.082.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid E. Rayyan – a web and mobile app for systematic reviews. Syst Rev. 2026;5:210.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses [Internet]. Ottawa: Ottawa Hospital Research Institute; 2011 [cited 2024 March 6]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm.
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis. Adelaide, Australia: JBI, 2020. Available from: https://synthesismanual.jbi.global.
Eickhoff SB, Bzdok D, Laird AR, Kurth F, Fox PT. Activation likelihood estimation meta-analysis revisited. Neuroimage. 2012;59:2349–61.
Eickhoff SB, Laird AR, Grefkes C, Wang LE, Zilles K, Fox PT. Coordinate‐based activation likelihood estimation meta‐analysis of neuroimaging data: a random‐effects approach based on empirical estimates of spatial uncertainty. Hum Brain Mapp. 2009;30:2907–26.
Turkeltaub PE, Eickhoff SB, Laird AR, Fox M, Wiener M, Fox P. Minimizing within‐experiment and within‐group effects in activation likelihood estimation meta‐analyses. Hum Brain Mapp. 2011;33:1–13.
Cheng B, Zhou Y, Kwok VPY, Li Y, Wang S, Zhao Y, et al. Altered functional connectivity density and couplings in postpartum depression with and without anxiety. Soc Cogn Affect Neurosci. 2021;17:756–66.
Cheng B, Wang X, Roberts N, Zhou Y, Wang S, Deng P, et al. Abnormal dynamics of resting-state functional activity and couplings in postpartum depression with and without anxiety. Cereb Cortex. 2022;32:5597–608.
Chen K, Yang J, Li F, Chen J, Chen M, Shao H, et al. Molecular basis underlying default mode network functional abnormalities in postpartum depression with and without anxiety. Hum Brain Mapp. 2024;45:e26657.
Eickhoff SB, Nichols TE, Laird AR, Hoffstaedter F, Amunts K, Fox PT, et al. Behavior, sensitivity, and power of activation likelihood estimation characterized by massive empirical simulation. NeuroImage. 2016;137:70–85.
Siddiqi SH, Taylor SF, Cooke D, Pascual-Leone A, George MS, Fox MD. Distinct symptom-specific treatment targets for circuit-based neuromodulation. Am J Psychiatry. 2020;177:435–46. https://doi.org/10.1176/appi.ajp.2019.19090915.
Long X, Zhou Y, Zhang F, Li F, Wang X, Meng Y, et al. Altered MRI diffusion properties of the white matter tracts connecting frontal and thalamic brain regions in first-episode, drug-naïve patients with postpartum depression. J Magn Reson Imaging. 2023;57:899–906.
Sasaki Y, Ito K, Fukumoto K, Kawamura H, Oyama R, Sasaki M, et al. Cerebral diffusion kurtosis imaging to assess the pathophysiology of postpartum depression. Sci Rep. 2020;10:15391.
Silver M, Moore CM, Villamarin V, Jaitly N, Hall JE, Rothschild AJ, et al. White matter integrity in medication-free women with peripartum depression: a tract-based spatial statistics study. Neuropsychopharmacology. 2018;43:1573–80.
Chen C, Li B, Zhang S, Liu Z, Wang Y, Xu M, et al. Aberrant structural and functional alterations in postpartum depression: a combined voxel-based morphometry and resting-state functional Connectivity study. Front Neurosci. 2023;17:1138561.
Cheng B, Hu X, Roberts N, Zhao Y, Xu X, Zhou Y, et al. Prolactin mediates the relationship between regional gray matter volume and postpartum depression symptoms. J Affect Disord. 2022;301:253–9.
Hare MM, Barber A, Shaffer SA, Deligiannidis KM. Bidirectional associations between perinatal allopregnanolone and depression severity with postpartum gray matter volume in adult women. Acta Psychiatr Scand. 2024;150:404–15.
Huang X, Zhuo Y, Wang X, Xu J, Yang Z, Zhou Y, et al. Structural and functional improvement of amygdala sub-regions in postpartum depression after acupuncture. Front Hum Neurosci. 2023;17:1163746.
Li Y, Chu T, Che K, Dong F, Shi Y, Ma H, et al. Abnormalities of cortical structures in patients with postpartum depression: a surface-based morphometry study. Behav Brain Res. 2021;410:113340.
Li Y, Chu T, Che K, Dong F, Shi Y, Ma H, et al. Altered gray matter structural covariance networks in postpartum depression: a graph theoretical analysis. J Affect Disord. 2021;293:159–67.
Yang W, Jiang Y, Ma L, Xiao M, Liu M, Ren Z, et al. Cortical and subcortical morphological alterations in postpartum depression. Behav Brain Res. 2023;447:114414.
Chase HW, Moses-Kolko EL, Zevallos C, Wisner KL, Phillips ML. Disrupted posterior cingulate–amygdala connectivity in postpartum depressed women as measured with resting BOLD fMRI. Soc Cogn Affect Neurosci. 2014;9:1069–75.
Che K, Mao N, Li Y, Liu M, Ma H, Bai W, et al. Altered spontaneous neural activity in peripartum depression: a resting-state functional magnetic resonance Imaging study. Front. Psychol. 2020;11:656.
Cheng B, Roberts N, Zhou Y, Wang X, Li Y, Chen Y, et al. Social support mediates the influence of cerebellum functional connectivity strength on postpartum depression and postpartum depression with anxiety. Transl Psychiatry. 2022;12:1–7.
Cheng B, Meng Y, Zhou Y, Li J, Zeng J, Tan X, et al. Cerebral regional homogeneity alternation of pregnant women with antenatal depression during the pandemic. Front Psychiatry. 2021;12:627871.
Cheng B, Wang X, Zhou Y, Li J, Zhao Y, Xia S, et al. Regional cerebral activity abnormality in pregnant women with antenatal depression. J Affect Disord. 2020;274:381–8.
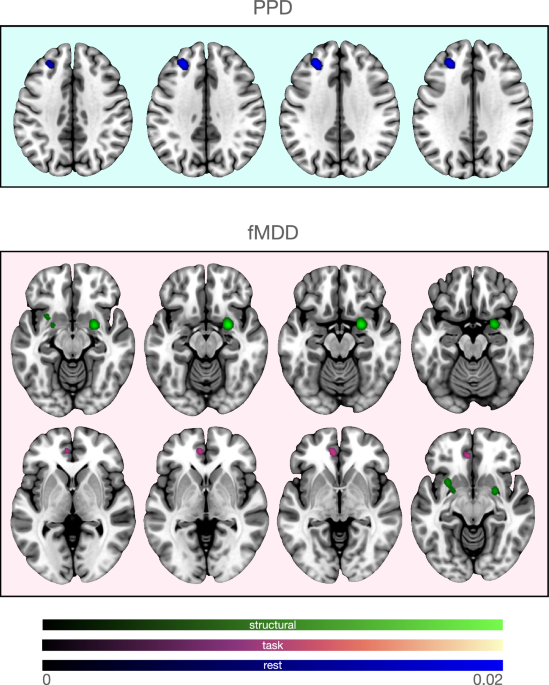
Cheng B, Guo Y, Chen X, Lv B, Liao Y, Qu H, et al. Postpartum depression and major depressive disorder: the same or not? Evidence from resting-state functional MRI. Psychoradiology. 2022;2:121–8.
Dong F, Zhang Z, Chu T, Che K, Li Y, Gai Q, et al. Altered dynamic amplitude of low-frequency fluctuations in patients with postpartum depression. Behav Brain Res. 2022;433:113980.
Deligiannidis KM, Sikoglu EM, Shaffer SA, Frederick B, Svenson A, Kopoyan A, et al. GABAergic neuroactive steroids and resting-state functional connectivity in postpartum depression: a Preliminary study. J Psychiatr Res. 2013;47:816–28.
Deligiannidis KM, Fales CL, Kroll-Desrosiers AR, Shaffer SA, Villamarin V, Tan Y, et al. Resting-state functional connectivity, cortical GABA, and neuroactive steroids in peripartum and peripartum depressed women: a functional magnetic resonance imaging and spectroscopy study. Neuropsychopharmacology. 2019;44:546–54.
Li B, Zhang S, Li S, Liu K, Hou X. Aberrant resting-state regional activity in patients with postpartum depression. Front Hum Neurosci. 2023;16:925543.
Mao N, Che K, Xie H, Li Y, Wang Q, Liu M, et al. Abnormal information flow in postpartum depression: a resting-state functional magnetic resonance imaging study. J Affect Disord. 2020;277:596–602.
Xiao-juan W, Jian W, Zhi-hong L, Yan M, Shi-Wei Z. Increased posterior cingulate, medial frontal and decreased temporal regional homogeneity in depressed mothers. A resting-state functional magnetic resonance study. Procedia Environ Sci. 2011;8:737–43.
Xu J, Yu H, Lv H, Zhou Y, Huang X, Xu Y, et al. Consistent functional abnormalities in patients with postpartum depression. Behav Brain Res. 2023;450:114467.
Zhang Y, Mu Y, Li X, Sun C, Ma X, Li S, et al. Improved interhemispheric functional connectivity in postpartum depression disorder: associations with individual target-transcranial magnetic stimulation treatment effects. Front Psychiatry. 2022;13:859453.
Zhang S, Li B, Liu K, Hou X, Zhang P. Abnormal voxel-based degree centrality in patients with postpartum depression: a resting-state functional magnetic resonance imaging study. Front Neurosci. 2022;16:914894.
Zhang S, Wang W, Wang G, Li B, Chai L, Guo J, et al. Aberrant resting-state interhemispheric functional connectivity in patients with postpartum depression. Behav Brain Res. 2020;382:112483.
Dudin A, Wonch KE, Davis AD, Steiner M, Fleming AS, Hall GB. Amygdala and affective responses to infant pictures: Comparing depressed and non-depressed mothers and non-mothers. J Neuroendocrinol. 2019;31:e12790.
Finnegan MK, Kane S, Heller W, Laurent H. Mothers’ neural response to valenced infant interactions predicts postpartum depression and anxiety. PLOS ONE. 2021;16:e0250487.
Lenzi D, Trentini C, Macaluso E, Graziano S, Speranza AM, Pantano P, et al. Mothers with depressive symptoms display differential brain activations when empathizing with infant faces. Psychiatry Res Neuroimaging. 2016;249:1–11.
Moses-Kolko EL, Fraser D, Wisner KL, James JA, Saul AT, Fiez JA, et al. Rapid habituation of ventral striatal response to reward receipt in postpartum depression. Biol Psychiatry. 2011;70:395–9.
Moses-Kolko EL, Perlman SB, Wisner KL, James J, Saul AT, Phillips ML. Abnormally reduced dorsomedial prefrontal cortical activity and effective connectivity with amygdala in response to negative emotional faces in postpartum depression. Am J Psychiatry. 2010;167:1373–80.
Silverman ME, Loudon H, Liu X, Mauro C, Leiter G, Goldstein MA. The neural processing of negative emotion postpartum: a preliminary study of amygdala function in postpartum depression. Arch Womens Ment Health. 2011;14:355–9.
Wonch KE, de Medeiros CB, Barrett JA, Dudin A, Cunningham WA, Hall GB, et al. Postpartum depression and brain response to infants: differential amygdala response and connectivity. Soc Neurosci. 2016;11:600–17.
Morgan JK, Santosa H, Fridley RM, Conner KK, Hipwell AE, Forbes EE, et al. Postpartum depression is associated with altered neural connectivity between affective and mentalizing regions during mother-infant interactions. Front Glob Womens Health. 2021;2:744649.
Song Z, Zhou Y, Zheng Y, Huang W, Meng Z, Li H, et al. Factors influencing functional near-infrared spectroscopy in postpartum depression: a cross-sectional study. Int J Gynecol Obstet. 2023;161:1046–52.
de Rezende MG, Rosa CE, Garcia-Leal C, de Figueiredo FP, Cavalli RdeC, et al. Correlations between changes in the hypothalamic-pituitary-adrenal axis and neurochemistry of the anterior cingulate gyrus in postpartum depression. J Affect Disord. 2018;239:274–81.
Epperson CN, Gueorguieva R, Czarkowski KA, Stiklus S, Sellers E, Krystal JH, et al. Preliminary evidence of reduced occipital GABA concentrations in puerperal women: a 1H-MRS study. Psychopharmacology. 2006;186:425–33.
McEwen AM, Burgess DTA, Hanstock CC, Seres P, Khalili P, Newman SC, et al. Increased glutamate levels in the medial prefrontal cortex in patients with postpartum depression. Neuropsychopharmacology. 2012;37:2428–35.
Rosa CE, Soares JC, Figueiredo FP, Cavalli RC, Barbieri MA, Schaufelberger MS, et al. Glutamatergic and neural dysfunction in postpartum depression using magnetic resonance spectroscopy. Psychiatry Res Neuroimaging. 2017;265:18–25.
Sacher J, Rekkas PV, Wilson AA, Houle S, Romano L, Hamidi J, et al. Relationship of Monoamine Oxidase-A distribution volume to postpartum depression and postpartum crying. Neuropsychopharmacology. 2015;40:429–35.
Moses-Kolko EL, Price JC, Wisner KL, Hanusa BH, Meltzer CC, Berga SL, et al. Postpartum and depression status are associated with lower [11C]raclopride BPND in reproductive-age women. Neuropsychopharmacology. 2012;37:1422–32.
Domain L, Guillery M, Linz N, König A, Batail JM, David R, et al. Multimodal MRI cerebral correlates of verbal fluency switching and its impairment in women with depression. Neuroimage Clin. 2022;33:102910.
Lyon M, Welton T, Varda A, Maller JJ, Broadhouse K, Korgaonkar MS, et al. Gender-specific structural abnormalities in major depressive disorder revealed by fixel-based analysis. Neuroimage Clin. 2019;21:101668.
Carceller-Sindreu M, de Diego-Adeliño J, Serra-Blasco M, et al. Volumetric MRI study of the habenula in first episode, recurrent and chronic major depression. Eur Neuropsychopharmacol. 2015;25:2015–21.
Depping MS, Wolf ND, Vasic N, Sambataro F, Thomann PA, Christian Wolf R. Specificity of abnormal brain volume in major depressive disorder: a comparison with borderline personality disorder. J Affect Disord. 2015;174:650–7.
Hastings RS, Parsey RV, Oquendo MA, Arango V, Mann JJ. Volumetric analysis of the prefrontal cortex, amygdala, and hippocampus in major depression. Neuropsychopharmacology. 2004;29:952–9.
Hu X, Zhang L, Liang K, Cao L, Liu J, Li H, et al. Sex-specific alterations of cortical morphometry in treatment-naïve patients with major depressive disorder. Neuropsychopharmacology. 2022;47:2002–9.
Kim MJ, Hamilton JP, Gotlib IH. Reduced caudate gray matter volume in women with major depressive disorder. Psychiatry Res. 2008;164:114–22.
Kong L, Chen K, Womer F, Jiang W, Luo X, Driesen N, et al. Sex differences of gray matter morphology in cortico-limbic-striatal neural system in major depressive disorder. J Psychiatr Res. 2013;47:733–9.
Mak AKY, Wong MMC, Han Shui, Lee TMC. Gray matter reduction associated with emotion regulation in female outpatients with major depressive disorder: a voxel-based morphometry study. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:1184–90.
Siragusa MA, Rufin T, Courtois R, Belzung C, Andersson F, Brizard B, et al. Left amygdala volume and brain tissue pulsatility are associated with neuroticism: an MRI and Ultrasound study. Brain Imaging Behav. 2021;15:1499–507.
Tang Y, Wang F, Xie G, Liu J, Li L, Su L, et al. Reduced ventral anterior cingulate and amygdala volumes in medication-naïve females with major depressive disorder: a voxel-based morphometric magnetic resonance imaging study. Psychiatry Res Neuroimaging. 2007;156:83–6.
Yang X, Peng Z, Ma X, Meng Y, Li M, Zhang J, et al. Sex differences in the clinical characteristics and brain gray matter volume alterations in unmedicated patients with major depressive disorder. Sci Rep. 2017;7:2515.
Yang J, Yin Y, Svob C, Long J, He X, Zhang Y, et al. Amygdala atrophy and its functional disconnection with the cortico-striatal-pallidal-thalamic circuit in major depressive disorder in females. PLoS ONE. 2017;12:e0168239.
Amiri S, Arbabi M, Kazemi K, Parvaresh-Rizi M, Mirbagheri MM. Characterization of brain functional connectivity in treatment-resistant depression. Prog Neuropsychopharmacol Biol Psychiatry. 2021;111:110346.
Belleau EL, Bolton TAW, Kaiser RH, Clegg R, Cárdenas E, Goer F, et al. Resting state brain dynamics: associations with childhood sexual abuse and major depressive disorder. Neuroimage Clin. 2022;36:103164.
Chen J, Luo Q, Li Y, Wu Z, Lin X, Yao J, et al. Intrinsic brain abnormalities in female major depressive disorder patients with childhood trauma: a resting-state functional magnetic resonance imaging study. Front Neurosci. 2022;16:930997.
Dong D, Pizzagalli DA, Bolton TAW, Ironside M, Zhang X, Li C, et al. Sex-specific resting state brain network dynamics in patients with major depressive disorder. Neuropsychopharmacology. 2024;49:806–13.
Li GZ, Liu PH, Zhang AX, Andari E, Zhang KR. A resting state fMRI study of major depressive disorder with and without anxiety. Psychiatry Res. 2022;315:114697.
Mei L, Wang Y, Liu C, Mou J, Yuan Y, Qiu L, et al. Study of sex differences in unmedicated patients with major depressive disorder by using resting state brain functional magnetic resonance imaging. Front Neurosci. 2022;16:814410.
Pessin S, Walsh EC, Hoks RM, Birn RM, Abercrombie HC, Philippi CL. Resting-state neural signal variability in women with depressive disorders. Behav Brain Res. 2022;433:113999.
Philippi CL, Leutzinger K, Pessin S, Cassani A, Mikel O, Walsh EC, et al. Neural signal variability relates to maladaptive rumination in depression. J Psychiatr Res. 2022;156:570–8.
Sun J, Luo Y, Ma Y, Guo C, Du Z, Gao S, et al. Sex differences of the functional brain activity in treatment-resistant depression: a resting-state functional magnetic Resonance Study. Brain Sci. 2022;12:1604.
Tang Y, Zhang X, Sheng J, Zhang X, Zhang J, Xu J, et al. Elevated hippocampal choline level is associated with altered functional connectivity in females with major depressive disorder: A pilot study. Psychiatry Res Neuroimaging. 2018;278:48–55.
Teng C, Zhou J, Ma H, Tan Y, Wu X, Guan C, et al. Abnormal resting state activity of left middle occipital gyrus and its functional connectivity in female patients with major depressive disorder. BMC Psychiatry. 2018;18:370.
Tu Z, Wu F, Jiang X, Kong L, Tang Y. Gender differences in major depressive disorders: a resting state fMRI study. Front Psychiatry. 2022;13:1025531.
Zhang X, Tang Y, Maletic-Savatic M, Sheng J, Zhang X, Zhu Y, et al. Altered neuronal spontaneous activity correlates with glutamate concentration in medial prefrontal cortex of major depressed females: an fMRI-MRS study. J Affect Disord. 2016;201:153–61.
Abler B, Erk S, Herwig U, Walter H. Anticipation of aversive stimuli activates extended amygdala in unipolar depression. J Psychiatr Res. 2007;41:511–22.
Almeida JR, Kronhaus DM, Sibille EL, Langenecker SA, Versace A, Labarbara E. Abnormal left-sided orbitomedial prefrontal cortical-amygdala connectivity during happy and fear face processing: a potential neural mechanism of female MDD. Front Psychiatry. 2011;2:69.
Baeken C, Van Schuerbeek P, De Raedt R, Ramsey NF, Bossuyt A, De Mey J. Reduced left subgenual anterior cingulate cortical activity during withdrawal-related emotions in melancholic depressed female patients. J Affect Disord. 2010;127:326–31.
Bär KJ, Wagner G, Koschke M, Boettger S, Boettger MK, Schlösser R, et al. Increased prefrontal activation during pain perception in major depression. Biol Psychiatry. 2007;62:1281–7.
Briceño EM, Weisenbach SL, Rapport LJ, Hazlett KE, Bieliauskas LA, Haase BD, et al. Shifted inferior frontal laterality in women with major depressive disorder is related to emotion-processing deficits. Psychol Med. 2013;43:1433–45.
Briceño EM, Rapport LJ, Kassel MT, Bieliauskas LA, Zubieta JK, Weisenbach SL. Age and gender modulate the neural circuitry supporting facial emotion processing in adults with major depressive disorder. Am J Geriatr Psychiatry. 2015;23:304–13.
Cane C, Carcone D, Gardhouse K, Lee ACH, Ruocco AC. An exploratory study of functional brain activation underlying response inhibition in major depressive disorder and borderline personality disorder. PLoS One. 2023;18:e0280215.
Dong D, Ironside M, Belleau EL, Sun X, Cheng C, Xiong G, et al. Sex-specific neural responses to acute psychosocial stress in depression. Transl Psychiatry. 2022;12:2.
Ironside M, Moser AD, Holsen LM, Zuo CS, Du F, Perlo S, et al. Reductions in rostral anterior cingulate GABA are associated with stress circuitry in females with major depression: a multimodal imaging investigation. Neuropsychopharmacology. 2021;46:2188–96.
Kumari V, Mitterschiffthaler MT, Teasdale JD, Malhi GS, Brown RG, Giampietro V, et al. Neural abnormalities during cognitive generation of affect in treatment-resistant depression. Biol Psychiatry. 2003;54:777–91.
Malejko K, Hafner S, Plener PL, Bonenberger M, Groen G, Abler B, et al. Neural signature of error processing in major depression. Eur Arch Psychiatry Clin Neurosci. 2021;271:1359–68.
Malejko K, Brown RC, Plener PL, Bonenberger M, Graf H, Abler B. Differential neural processing of unpleasant sensory stimulation in patients with major depression. Eur Arch Psychiatry Clin Neurosci. 2021;271:557–65.
Mitterschiffthaler MT, Kumari V, Malhi GS, Brown RG, Giampietro VP, Brammer MJ, et al. Neural response to pleasant stimuli in anhedonia: an fMRI study. NeuroReport. 2003;14:177.
Robert G, Bannier E, Comte M, Domain L, Corouge I, Dondaine T, et al. Multimodal brain imaging connectivity analyses of emotional and motivational deficits in depression among women. J Psychiatry Neurosci. 2021;46:E303–12.
Shao R, Zhang HJ, Lee TM. The neural basis of social risky decision making in females with major depressive disorder. Neuropsychologia. 2015;67:100–10.
Tak S, Lee S, Park CA, Cheong EN, Seok JW, Sohn JH, et al. Altered effective connectivity within the fronto-limbic circuitry in response to negative emotional task in female patients with major depressive disorder. Brain Connect. 2021;11:264–77.
Wagner G, Sinsel E, Sobanski T, Köhler S, Marinou V, Mentzel HJ, et al. Cortical inefficiency in patients with unipolar depression: an event-related fMRI study with the stroop task. Biol Psychiatry. 2006;59:958–65.
Young KD, Bodurka J, Drevets WC. Functional neuroimaging of sex differences in autobiographical memory recall in depression. Psychol Med. 2017;47:2640–52.
Yttredahl AA, McRobert E, Sheler B, Mickey BJ, Love TM, Langenecker SA, et al. Abnormal emotional and neural responses to romantic rejection and acceptance in depressed women. J Affect Disord. 2018;234:231–8.
Lyu H, Zhao M, Xu P, Li Y, Jiang C, Zhao H, et al. Gender differences in brain region activation during verbal fluency task as detected by fNIRS in patients with depression. World J Biol Psychiatry. 2024;25:141–50.
Ma XY, Wang YJ, Xu B, Feng K, Sun GX, Zhang XQ, et al. Near-infrared spectroscopy reveals abnormal hemodynamics in the left dorsolateral prefrontal cortex of menopausal depression patients. Dis Markers. 2017;2017:1695930.
Kantrowitz JT, Dong Z, Milak MS, Rashid R, Kegeles LS, Javitt DC, et al. Ventromedial prefrontal cortex/anterior cingulate cortex Glx, glutamate, and GABA levels in medication-free major depressive disorder. Transl Psychiatry. 2021;11:419.
Song Y, Cho JH, Kim H, Eum YJ, Cheong EN, Choi S, et al. Association between taurine level in the hippocampus and major depressive disorder in young women: a proton magnetic resonance Spectroscopy Study at 7T. Biol Psychiatry. 2024;95:465–72.
Tran KH, Luki J, Hanstock S, Hanstock CC, Seres P, Aitchison K, et al. The impact of matching for reproductive status on the comparison of magnetic spectroscopic measurements of glutamate and gamma-aminobutyric acid + in the medial prefrontal cortex of women with major depression. J Affect Disord. 2024;351:396–402.
Tran KH, Luki J, Hanstock S, Hanstock CC, Seres P, Aitchison K, et al. Decreased GABA+ ratios referenced to creatine and phosphocreatine in the left dorsolateral prefrontal cortex of females of reproductive age with major depression. J Psychiatry Neurosci. 2023;48:E285–E294.
Zhang Y, Han Y, Wang Y, Zhang Y, Li L, Jin E, et al. A MRS study of metabolic alterations in the frontal white matter of major depressive disorder patients with the treatment of SSRIs. BMC Psychiatry. 2015;15:99.
Zhong Q, Lai S, He J, Zhong S, Song X, Wang Y, et al. Gender-related alterations of serum trace elements and neurometabolism in the anterior cingulate cortex of patients with major depressive disorder. J Affect Disord. 2024;360:176–87.
Nugent AC, Bain EE, Thayer JF, Sollers JJ, Drevets WC. Heart rate variability during motor and cognitive tasks in females with major depressive disorder. Psychiatry Res Neuroimaging. 2011;191:1–8.
Williams LM, Goldstein-Piekarski AN (2020). Applying a neural circuit taxonomy in depression and anxiety for personalized psychiatry. In Baune BT (ed.), Personalized Psychiatry. London, UK: Elsevier Academic Press, 499–519.
Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. The Lancet Psychiatry. 2016;3:472–80.
Song EJ, Tozzi L, Williams LM. Brain circuit-derived biotypes for treatment selection in mood disorders: a critical review and illustration of a functional neuroimaging tool for clinical translation. Biol Psychiatry. 2024;96:552–63. https://doi.org/10.1016/j.biopsych.2024.03.016.
Tozzi L, Zhang X, Pines A, Olmsted AM, Zhai ES, Anene ET, et al. Personalized brain circuit scores identify clinically distinct biotypes in depression and anxiety. Nat Med. 2024;30:2076–87. https://doi.org/10.1038/s41591-024-03057-9.
Chesnut M, Harati S, Paredes P, Khan Y, Foudeh A, Kim J, et al. Stress markers for mental states and biotypes of depression and anxiety: a scoping review and preliminary illustrative analysis. Chronic Stress. 2021;5:24705470211000338.
Baez LM, Newport DJ, Stowe ZN, Knight BT, Heller AS. The severity and role of somatic depressive symptoms in psychological networks in a longitudinal sample of peripartum women. J Psychiatr Res. 2021;142:283–9.
Eid RS, Gobinath AR, Galea LAM. Sex differences in depression: insights from clinical and preclinical studies. Prog Neurobiol. 2019;176:86–102.
Tozzi L, Staveland B, Holt-Gosselin B, Chesnut M, Chang SE, Choi D, et al. The human connectome project for disordered emotional states: protocol and rationale for a research domain Criteria study of brain connectivity in young adult anxiety and depression. Neuroimage. 2020;214:116715.
Tozzi L, Goldstein-Piekarski AN, Korgaonkar MS, Williams LM. Connectivity of the cognitive control network during response inhibition as a predictive and response biomarker in major depression: evidence from a randomized clinical trial. Biol Psychiatry. 2020;87:462–72.
Coo S, García MI, Prieto F, Medina F. The role of interpersonal emotional regulation on maternal mental health. J Reprod Infant Psychol. 2022;40:3–21.
Cardoso C, Fonseca A. Mothers at-risk for postpartum depression: Mental health and emotion regulation throughout the postpartum period. Curr Psychol. 2023;42:12988–3002.
DeJong H, Fox E, Stein A. Rumination and postnatal depression: A systematic review and a cognitive model. Behav Res Ther. 2016;82:38–49.
Hack LM, Tozzi L, Zenteno S, Olmsted AM, Hilton R, Jubeir J, et al. A cognitive biotype of depression linking symptoms, behavior measures, neural circuits, and differential treatment outcomes: a prespecified secondary analysis of a randomized clinical trial. JAMA Netw Open. 2023;6:e2318411.
Petrošanec M, Brekalo M, Nakić Radoš S. The metacognitive model of rumination and depression in postpartum women. Psychol Psychother. 2022;95:838–52. https://doi.org/10.1111/papt.12405.
McTeague LM, Goodkind MS, Etkin A. Transdiagnostic impairment of cognitive control in mental illness. J Psychiatr Res. 2016;83:37–46.
O’Mahen H, Fedock G, Henshaw E, Himle JA, Forman J, Flynn HA. Modifying CBT for perinatal depression: What do women want?: a qualitative study. Cogn. Behav. Pract. 2012;19:359–71.
Bjertrup AJ, Jensen MB, Schjødt MS, Parsons CE, Kjærbye-Thygesen A, Mikkelsen RL, et al. Cognitive processing of infant stimuli in pregnant women with and without affective disorders and the association to postpartum depression. Eur Neuropsychopharmacol. 2021;42:97–109.
Webb R, Ayers S. Cognitive biases in processing infant emotion by women with depression, anxiety and post-traumatic stress disorder in pregnancy or after birth: a systematic review. Cogn Emot. 2015;29:1278–94.
Zhou HX, Chen X, Shen YQ, Li L, Chen NX, Zhu ZC, et al. Rumination and the default mode network: meta-analysis of brain imaging studies and implications for depression. Neuroimage. 2020;206:116287 https://doi.org/10.1016/j.neuroimage.2019.116287.
O’ Brien S, Sethi A, Gudbrandsen M, Lennuyeux-Comnene L, Murphy DGM, Craig MC. Is postnatal depression a distinct subtype of major depressive disorder? An exploratory study. Arch Womens Ment Health. 2021;24:329–33.
Putnam KT, Wilcox M, Robertson-Blackmore E, Sharkey K, Bergink V, Munk-Olsen T, et al. Clinical phenotypes of perinatal depression and time of symptom onset: analysis of data from an international consortium. Lancet Psychiatry. 2017;4:477–85.
Fox M, Sandman CA, Davis EP, Glynn LM. A longitudinal study of women’s depression symptom profiles during and after the postpartum phase. Depress Anxiety. 2018;35:292–304.
Bledsoe SE, Grote NK. Treating depression during pregnancy and the postpartum: a preliminary meta-analysis. Res. Soc. Work Pract. 2006;16:109–20.
De Crescenzo F, Perelli F, Armando M, Vicari S. Selective serotonin reuptake inhibitors (SSRIs) for post-partum depression (PPD): a systematic review of randomized clinical trials. J Affect Disord. 2014;152–154:39–44.
Kim DR, Epperson CN, Weiss AR, Wisner KL. Pharmacotherapy of postpartum depression: an update. Expert Opin Pharmacother. 2014;15:1223–34.
van Ravesteyn LM, Lambregtse – van den Berg MP, Hoogendijk WJG, Kamperman AM. Interventions to treat mental disorders during pregnancy: a systematic review and multiple treatment meta-analysis. PLoS ONE. 2017;12:e0173397.
Scangos KW, State MW, Miller AH, Baker JT, Williams LM. New and emerging approaches to treat psychiatric disorders. Nat Med. 2023;29:317–33.
Cole J, Bright K, Gagnon L, McGirr A. A systematic review of the safety and effectiveness of repetitive transcranial magnetic stimulation in the treatment of peripartum depression. J Psychiatr Res. 2019;115:142–50.
Pacheco F, Guiomar R, Brunoni AR, Buhagiar R, Evagorou O, Roca-Lecumberri A, et al. Efficacy of non-invasive brain stimulation in decreasing depression symptoms during the peripartum period: a systematic review. J Psychiatr Res. 2021;140:443–60.
Wang T, Wu H, Jiang Y, Huang W, Yu D, Zhang X, et al. Effects of rTMS in postpartum depression: a meta-analysis. J Nurse Pract. 2023;19:104488.
Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340:c221.