Summary of findings
To the best of our knowledge, this study provides the first comprehensive quantitative synthesis indicating a potential positive association between pre-existing cardiometabolic diseases and the future development of aggressive PCa. Looking further into the specific types of underlying conditions, diabetes exhibited the strongest association among all cardiometabolic conditions analyzed, with individuals with diabetes facing an 18% higher risk of developing aggressive PCa compared to non-diabetic counterparts. This finding stands out as the most pronounced risk elevation observed in the study, highlighting diabetes as a particularly important comorbidity that may deserve special attention in prostate cancer risk stratification and management efforts. Obesity followed closely, associated with a 15% increased risk of metastasis, reinforcing the growing recognition of adiposity as a driver of aggressive prostate cancer phenotypes [12, 42]. Hypertension was associated with a 7% increased risk of metastasis; however, this finding should be interpreted with caution given that the lower bound of the confidence interval touched the null value of 1.00, suggesting borderline statistical significance. Additionally, moderate heterogeneity (I2 = 51%) was observed, likely reflecting differences across studies in the definition and measurement of hypertension, participant characteristics (such as age, race, and disease severity), and inconsistent adjustment for potential confounders including obesity, smoking, and antihypertensive medication use. As suggested by prior research [43], differential effects of antihypertensive drug classes on prostate cancer progression may hold potential for influencing outcomes, although further studies are needed to establish these relationships more definitively. Potential mechanisms linking hypertension to metastasis, including inflammation, angiogenesis, and endothelial dysfunction, have been proposed [44, 45]. In contrast, the association between dyslipidemia and aggressive PCa was not statistically significant. It is notable that dyslipidemia was measured variably across studies—using indicators such as high LDL cholesterol, low HDL cholesterol, elevated triglycerides, or high total cholesterol—which may have contributed to inconsistency. Moreover, distinct biological mechanisms, such as the unique effects of lipid metabolism dysregulation on cellular pathways like Akt and mTOR, may further explain why dyslipidemia differs mechanistically from diabetes, hypertension, and obesity [46, 47]. The lack of a significant association underscores that not all cardiometabolic components contribute equally to aggressive PCa. This distinction is critical, as it highlights which comorbidities—specifically diabetes, obesity, and to a lesser extent hypertension—may warrant closer clinical surveillance or mechanistic investigation in the context of prostate cancer management.
Despite some modest effect sizes and observed heterogeneity, these findings carry meaningful clinical implications, particularly given the high global prevalence of cardiometabolic diseases among men at risk for prostate cancer with an estimated 3.3 million PCa survivors in the U.S. alone [1, 2]. Future studies with more uniform definitions of exposures and more detailed adjustment for key confounders, including pharmacologic treatments, are warranted to refine these associations and guide multidisciplinary strategies for risk stratification and intervention.
A comparison to prior meta-analyses helps contextualize the present findings. A meta-analysis conducted by the American Association for Cancer Research examined blood cholesterol levels and prostate cancer risk, finding no significant associations between total cholesterol, LDL, or HDL cholesterol and prostate cancer incidence or mortality [48]. These findings corroborate our result that dyslipidemia was not significantly associated with aggressive prostate cancer; however, our study specifically focused on advanced disease progression rather than overall incidence or mortality. A separate meta-analysis published by SpringerPlus in 2016, investigated the impact of diabetes mellitus on prostate cancer mortality, revealing a 29% increased risk of death among diabetic men, supporting our observation that diabetes is an important predictor of more aggressive prostate cancer outcomes [49]. Additionally, a systematic review and meta-analysis using the UK Biobank demonstrated that increased adiposity, particularly waist circumference and waist-to-hip ratio, was significantly associated with higher prostate cancer mortality, consistent with our finding that central obesity may be more predictive of aggressive disease than BMI alone [50]. Similarly, a dose–response meta-analysis found a positive association between higher BMI and prostate cancer mortality, reinforcing the relationship between general obesity and poor survival outcomes [51]. Furthermore, a meta-analysis identified hypertension as a modest but significant risk factor for prostate cancer, although their focus was on incidence rather than aggression, highlighting the novelty of our focus on disease progression [52]. Collectively, while prior meta-analyses established important links between cardiometabolic conditions and prostate cancer outcomes, our study is unique in its exclusive emphasis on aggressive prostate cancer and its integrated evaluation of multiple cardiometabolic risk factors, with Supplementary Table S4 providing a structured comparison of these differences.
Mechanistic effects
Several cardiometabolic diseases may contribute to aggressive prostate cancer through overlapping biological mechanisms including chronic inflammation, immune cell activation, hormonal imbalances, and metabolic dysregulation.
Chronic inflammation is a recognized biological driver of cancer progression and metastasis, including in PCa. Persistent low-grade inflammation disrupts tissue homeostasis, facilitates DNA damage, and modulates the tumor microenvironment, all of which contribute to tumor progression and dissemination. In particular, inflammation of the vascular endothelium fosters a permissive environment for tumor invasion and angiogenesis — key steps in metastasis [47, 53, 54]. This is notably exacerbated in individuals with obesity, where excess adipose tissue acts as a potent source of pro-inflammatory cytokines such as IL-6, TNF-α, and leptin, which have been shown to enhance tumor cell proliferation, migration, and immune evasion [47, 55, 56].
Importantly, the normal prostate gland expresses high levels of insulin receptors, making it particularly responsive to metabolic changes [42]. In type 2 diabetes mellitus, hyperinsulinemia and elevated insulin-like growth factor 1 (IGF-1) levels drive activation of the PI3K/Akt/mTOR pathway, enhancing cell survival and proliferation [57]. These hormonal shifts also suppress immune surveillance via increased cortisol and adrenal steroid synthesis, facilitating immune evasion and tumor progression [57]. Additionally, insulin resistance further intensifies systemic inflammation, creating a feedback loop that promotes tumorigenic processes [58, 59]. PCa cells have been shown to overexpress insulin receptors, and exposure to diabetogenic insulin and glucose concentrations in vitro enhances their migratory, adhesive, and proliferative capacity [60].
Obesity, especially when induced by a high-fat diet, influences metastatic PCa through hormonal, immunologic, and metabolic pathways. Excess adiposity increases aromatase activity, leading to elevated systemic estrogen levels, which interact with estrogen receptors (ERs) frequently expressed in advanced prostate tumors [42, 55]. This promotes tumor cell proliferation and cross-talk between ER and AR signaling pathways [55]. Obesity also drives infiltration of macrophages into periprostatic adipose tissue, where they secrete IL-6. This cytokine has a dual role—facilitating both inflammatory signaling and androgen receptor (AR) activation, contributing directly to PCa cell proliferation, epithelial–mesenchymal transition, and metastasis [46]. In clinical and experimental studies, elevated IL-6 levels correlate with more aggressive disease and higher mortality in PCa patients [61]. Furthermore, AR overexpression in prostate tumors from diabetic individuals suggests that metabolic stress augments hormone sensitivity and metastatic potential [62]. Notably, WC—a measure of central adiposity—may offer a more precise link to metastatic risk than BMI alone. WC reflects visceral fat, which is metabolically more active than subcutaneous fat and secretes pro-tumorigenic cytokines including leptin, TNF-α, and IL-6, all of which promote a pro-metastatic tumor microenvironment [55]. Elevated WC has been independently associated with advanced-stage PCa and higher mortality, potentially through paracrine signaling that facilitates tumor invasiveness and systemic endocrine disruption [55]. These data suggest that regional fat distribution may be a key mechanistic driver of disease progression, and not just total body mass.
There is strong mechanistic overlap between IL-6 signaling, type 2 diabetes, and obesity, particularly through the activation of STAT3 and AR pathways. Elevated systemic IL-6, commonly observed in both obese and diabetic individuals, has been linked to high-grade PCa and increased androgen receptor sensitivity [46, 54, 55]. These shared inflammatory and hormonal axes provide a robust explanation for our observed associations between metabolic dysregulation and aggressive PCa.
In contrast, the mechanisms linking dyslipidemia to aggressive PCa are less inflammatory and more centered on lipid signaling and cholesterol metabolism. Dyslipidemia alters membrane lipid raft composition, affecting receptor clustering and intracellular signaling [47]. Elevated serum cholesterol facilitates de novo steroidogenesis and enhances AR activation, thus sustaining PCa growth in androgen-depleted conditions [46, 47]. Activated Akt, a kinase essential to prostate cancer growth and progression, has been strongly associated with hypercholesterolemia, PC3 cell proliferation, and increased intratumoral androgen production [63]. These effects underscore the role of cholesterol as more than a passive metabolic factor—it is a key modulator of prostate cancer cell behavior. While inflammation is not the central mechanism in dyslipidemia, its metabolic effects may interact with other cardiometabolic conditions—particularly obesity and diabetes—to exacerbate androgen signaling, tumor cell migration, and metabolic adaptation within the tumor microenvironment [64]. While the association between dyslipidemia and aggressive PCa was not statistically significant in our meta-analysis, this likely reflects the heterogeneity of underlying mechanisms rather than the absence of biological relevance. These findings emphasize the need for disease-specific mechanistic research, as not all cardiometabolic comorbidities contribute equally to cancer aggressiveness.
Hypertension contributes to metastatic potential through mechanical and oxidative stress. Repeated high-pressure states result in vascular remodeling, activating enzymes like matrix metalloproteinase-2 (MMP-2), which degrade the extracellular matrix (ECM) and facilitate cancer cell invasion [44, 45]. Furthermore, endothelial dysfunction, a hallmark of chronic hypertension, promotes angiogenesis, inflammation, and loss of vascular integrity—key steps for tumor cell intravasation and extravasation during metastasis [45]. Studies consistently report upregulated MMP-2 expression and neovascularization in hypertensive individuals, supporting the mechanistic plausibility of this association. Angiogenesis is a common mechanistic denominator in many of these pathways: the formation of new blood vessels not only supports tumor growth, but also provides a route for prostate cancer cells to spread to distant tissues [45].
The present findings reinforce the hypothesis that cardiometabolic dysfunction, particularly diabetes and obesity, are major drivers of prostate cancer aggressiveness. Diabetes was associated with an 18% increased risk of aggressive PCa, while obesity contributed a 15% increased risk, underscoring their clinical relevance. Mechanistically, both conditions converge on shared pathways such as chronic inflammation, hyperinsulinemia, immune suppression, and activation of pro-metastatic signaling cascades including PI3K/Akt/mTOR [65,66,67]. The role of vascular dysfunction, driven by metabolic syndrome components, further enhances tumor invasion and metastatic potential, as supported by PSA variability and disease severity in hypertensive patients [68]. Notably, Tanaka and Node (2019) emphasized that cardiometabolic syndrome is not merely a comorbidity but an active facilitator of prostate cancer progression, a view strongly aligned with our results [69]. Collectively, these data support an emerging paradigm where integrated metabolic control may be critical not only for cardiovascular outcomes but also for mitigating prostate cancer aggressiveness.
Strengths and limitations
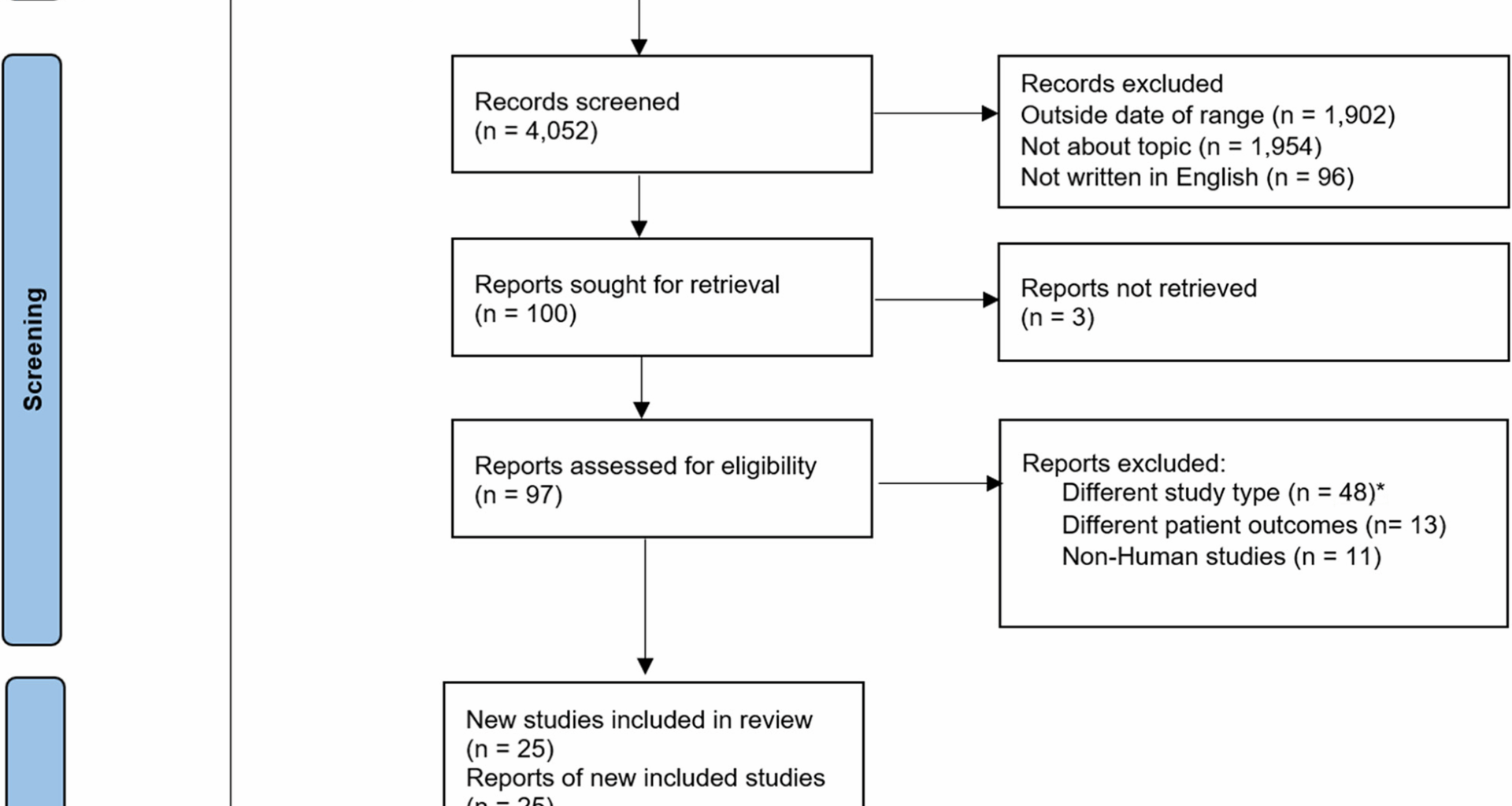
The major strengths of this study are its objectivity and rigor. Regarding objectivity, following standardized procedures not only minimized the influence of personal biases but aided in validity for the findings through consistent data collection. Such a method encourages repeatability and openness, as every stage of the review process was methodically recorded and reported. Data analyses were conducted equitably and without preference for any specific result. As for the rigor of the study, a clear research design that adhered to PRISMA guidelines was used, and explicit inclusion and exclusion criteria were applied to each and every study that was reviewed. Risk of bias was assessed using the Newcastle–Ottawa Scale, and results are included in the supplementary material as Supplementary Table S2.
On the other hand, this systematic review and meta-analysis is limited by the scarcity and heterogeneity of studies, in turn affecting the robustness and reliability of the findings. The high levels of heterogeneity observed in this study suggest that differences in study methods, populations, outcome definitions, and exposure assessments may have influenced the consistency of reported associations. Most included studies assessed cardiometabolic risk factors through clinical examination, biomarker data, or registry coding. However, two studies relied on self-reported diabetes status, which may introduce recall or misclassification bias. Importantly, the average follow-up period across all studies was 9.8 years, which supports a temporal relationship between cardiometabolic exposures and prostate cancer outcomes and helps mitigate concerns regarding reverse causality. The long lag time also suggests that measured risk factors likely preceded diagnosis in most cases. Additionally, the average cohort size was 38,990 participants, providing sufficient power across studies, although a few included relatively small subsets of patients with advanced or metastatic disease, which may impact the precision of effect estimates. Stratification by study size and follow-up time had also been performed to further assess heterogeneity. The overall findings remained consistent across large and small studies, reducing concerns about small-study bias. A modest gradient in HRs was observed across follow-up time categories, which may reflect latency in prostate cancer progression. However, due to limited availability of retrospective studies and non-clinical exposure definitions, we did not perform subgroup analyses for study design or exposure source.
Additionally, the literature search for this meta-analysis was conducted exclusively through PubMed. While PubMed is a comprehensive and widely-used biomedical database, restricting the search to a single source may have resulted in the omission of relevant studies indexed only in other databases such as Embase, Scopus, or the Cochrane Library. Although manual reference tracking was performed to identify additional eligible studies, this limitation could affect the overall comprehensiveness and generalizability of the review. The complete search strategy has been provided in Supplementary Table S1 for transparency and reproducibility.
Visual inspection of funnel plots revealed moderate asymmetry in several analyses, particularly for obesity and diabetes, suggesting a potential publication bias favoring studies with statistically significant findings. This asymmetry raises concerns about selective reporting and the possible underrepresentation of null or inverse results in the literature. As a result, the strength of some pooled estimates may be inflated, which impacts the generalizability and interpretability of these associations. While formal statistical tests for publication bias were limited due to the number of studies in some subgroups, the patterns observed underscore the need for greater transparency and pre-registration of observational studies in this field.
Another limitation to consider is detection bias, particularly among obese individuals. Higher body mass has been associated with hemodilution of serum PSA levels, which may delay diagnosis and result in underrepresentation of early-stage cases. This could create the appearance of stronger associations between obesity and advanced disease, even when no such biological link exists. Furthermore, collider stratification bias is a potential concern. Since cardiometabolic conditions like diabetes or obesity may influence both the risk of developing prostate cancer and the probability of detection, restricting the analysis to individuals with diagnosed cancer may introduce spurious associations. These types of bias are difficult to correct for in meta-analytic frameworks, but they warrant caution when interpreting associations as causal.
In addition, several of the original studies reported hazard ratios with confidence intervals that crossed 1, indicating that these individual results could not exclude the possibility of no statistically significant difference between the exposed and control groups. This adds further uncertainty to the synthesized estimates, particularly in cases where the pooled result may be influenced by a few larger or more extreme studies. A major limitation is that there were too few studies (n = 2) that stratified by race to draw any meaningful conclusions regarding differential associations with aggressive PCa, despite general scientific awareness of the disparities in PCa incidence and outcomes suffered by Black men compared to Whites.
Finally, we acknowledge the potential impact of residual confounding and survival bias. Although multivariable-adjusted estimates were prioritized where available, unmeasured or inconsistently reported variables—such as socioeconomic status, dietary intake, physical activity, and access to healthcare—could influence both the presence of cardiometabolic disease and prostate cancer progression, thereby introducing bias. Additionally, survival bias may be relevant, as individuals with severe cardiometabolic disease may experience premature mortality from non-cancer causes, potentially before metastatic progression is diagnosed. As discussed by Dilixiati et al. [70], such bias can obscure or attenuate the true associations between exposure and cancer outcomes, particularly in older or high-risk populations.
Public health implications and future research
The possible conjunction of diabetes, hypertension, and obesity as contributors to aggressive PCa carries profound public health implications, resonating across clinical practice, research endeavors, and the fields of oncology and cardiology. Should these associations be corroborated in future studies, clinicians may gain greater awareness of the metastatic risks associated with cardiometabolic comorbidities and implement more tailored surveillance strategies for affected patients. Multidisciplinary care teams—including oncologists, urologists, obesity specialists, cardiologists, and primary care physicians—may be well-positioned to personalize treatment and monitoring regimens based on these risk profiles.
In particular, therapies aimed at improving cardiometabolic health have generated interest as potential adjuncts to standard prostate cancer treatment. While agents such as metformin have shown biologically plausible mechanisms—such as modulation of insulin signaling, mTOR inhibition, and anti-inflammatory effects—clinical evidence to date remains inconclusive. For example, the STAMPEDE trial found no survival advantage with the addition of metformin in men with metastatic prostate cancer, although it did reduce metabolic toxicity from androgen deprivation therapy [71]. Similarly, the MAST trial, evaluating metformin in low-risk prostate cancer during active surveillance, found no effect on disease progression [72]. A broader lifestyle intervention study also found no consistent evidence for dietary or metabolic agents significantly modifying prostate cancer outcomes, though improvements in quality of life and comorbidities were observed [73]. These findings suggest that while cardiometabolic therapies may not offer direct oncologic benefit in all settings, they could still play a supportive role in managing treatment-related side effects and comorbidity burden.
In the future, targeted surveillance and therapies could be informed through clarifying the underlying biological processes relating obesity, hypertension, and diabetes to the progression of PCa. Additional longitudinal cohort studies would be essential to validate the current literature and could also test for the effects of cardiometabolic therapies (i.e. pharmaceutical treatments and lifestyle changes) on cancer progression. Multidisciplinary cooperation between urologists, cardiologists, and oncologists, to name a few, can allow for comprehensive treatment plans in PCa patients with cardiometabolic comorbidities. Conducting research in medical systems such as the VA, that care for large numbers of African American men with prostate cancer would also contribute to a better understanding of the underlying disparities in incidence and mortality, especially given the high prevalence of cardiometabolic diseases in this group.
Although racial disparities are well-documented in prostate cancer outcomes, particularly among Black men, only two studies in our review stratified their findings by race [17, 40]. This limited our ability to evaluate differential associations. We highlight this as an important limitation and call for future cohort studies to routinely report and stratify findings by racial or ethnic groups to better understand population-specific risk patterns.