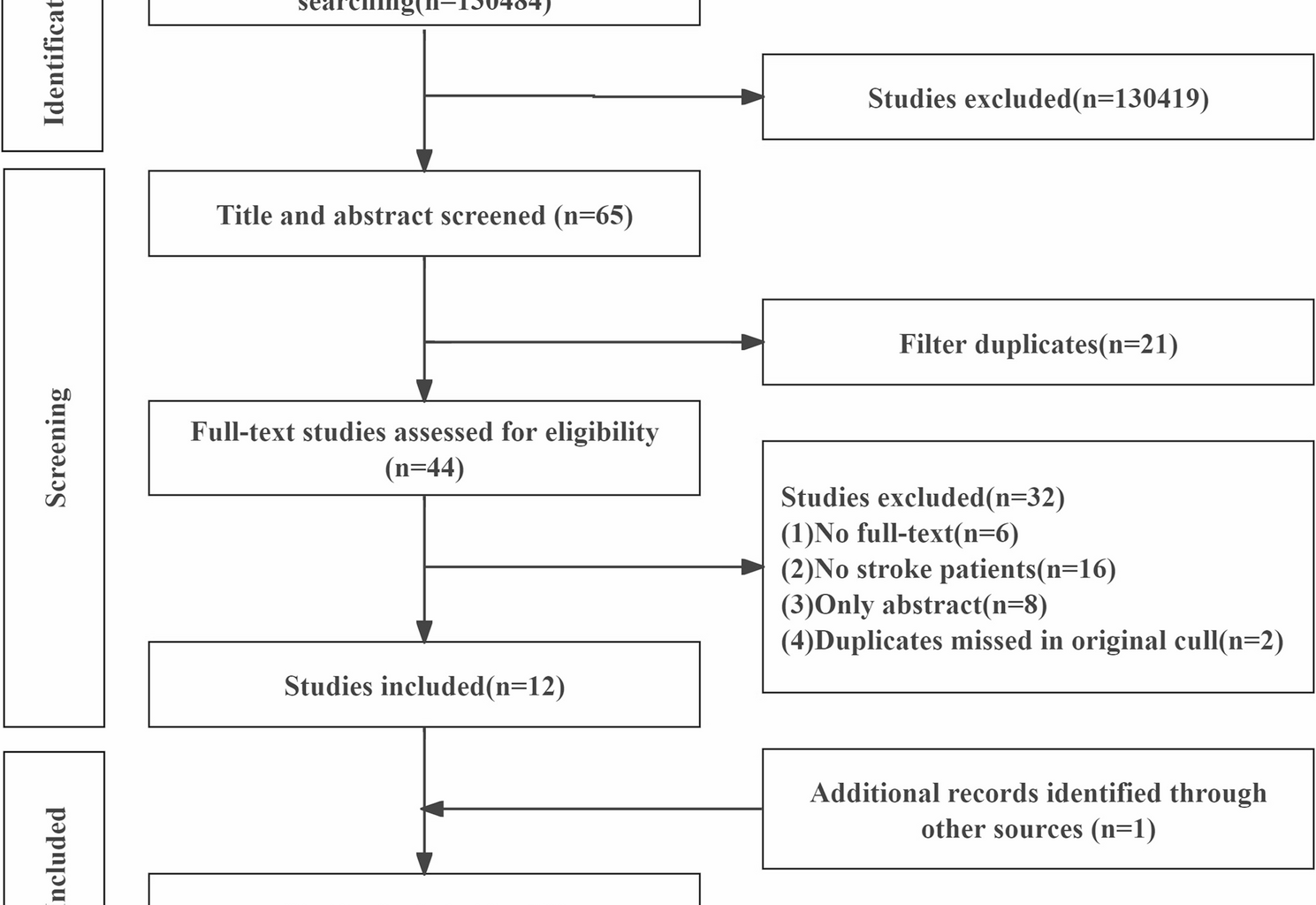
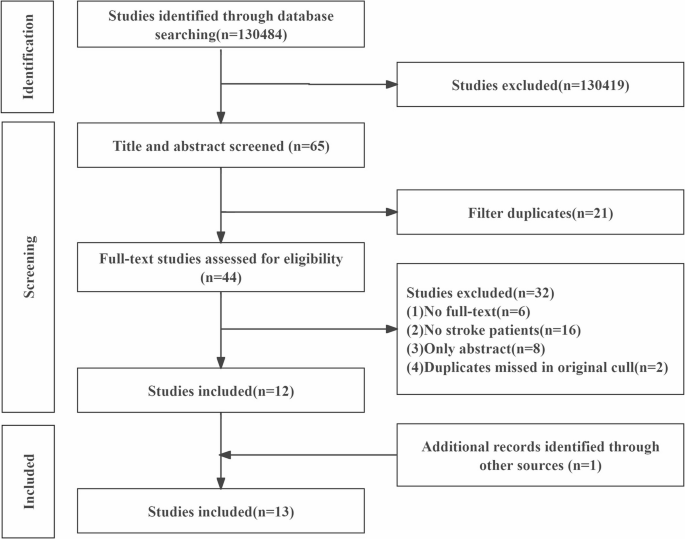
A total of 130,484 records were identified. After screening titles and abstracts and removing duplicates, 44 studies underwent full-text review, with 12 deemed eligible for analysis. Additionally, 1 eligible study was identified through manual references screening. Thus, 13 studies were included for the final analysis. The studies screening and selection process is illustrated in Fig. 1.
Flowchart of identification and screening of the included and excluded studies following the PRISMA 2020 guideline
Study characteristicsBaseline of the study
As presented in Table 2, the 13 studies were published between 2011 and 2024, originating from Hong Kong of China [32, 33], Japan [34,35,36,37], Turkey [38], Korea [39,40,41,42], Belgium [43], and France [44]. A total of 440 post-stroke patients, aged between 48.0 and 80.5, were investigated. Of the selected studies, 9 investigated inter-rater reliability and 9 assessed intra-rater reliability.
Table 2. Characteristics of the included studies [33,34,35,36,37,38,39,40,41,42,43,44]Ultrasound-based assessment
In these 13 studies, the gastrocnemius [33, 36, 39, 42,43,44] and tibialis anterior TA) [32, 40, 43, 44] were the most frequently studied. Other commonly examined muscles included the deltoid muscle [34], flexor digitorum superficialis and flexor digitorum profundus (FDS/FDP) [38], plantar fascia, abductor hallucis (AbH), flexor hallucis brevis (FHB), flexor digitorum brevis (FDB) [38], transversus abdominis, obliquus externus abdominis, obliquus internus abdominis [41], and supraspinatus [35], biceps brachii (BB) lateralis [37], vastus intermedius [37]. Additionally, muscle thickness MT) [32, 35,36,37, 40,41,42, 44, 45] were the most commonly analyzed parameter, followed by pennation angle (PA) [33, 39, 40, 42], muscle cross-sectional area (CSA) [33, 38, 45], muscle volume (MV) [43], and muscle length (ML) [43].
The 3D Ultrasound (frequency: 10 MHz) [43], Medison Mysono P-US system (frequency: 6‒14 MHz) [39], and 2D B-mode ultrasound (frequency: 7.5 MHz [32, 34, 40, 42], 6‒18 MHz [38], 4‒15 MHz [46], 10 MHz [33] 13 MHz [36, 37], and 12 MHz employed in the selected studies. A linear probe was utilized and positioned transversely for assessing MV [43], ML [33, 43], CSA [33, 38], MT [33, 35,36,37, 41, 44] and longitudinally for assessing MT [32, 34, 40, 42], PA [33, 36, 39, 40, 42], CSA [33]. A probe was commonly set at the origin over the muscle belly to the distal muscle-tendon junction of TA [43], the muscle bully of MG and TA [32], the midpoint of the joint between the later al acromion edge of the shoulder peak and deltoid tuberosity of deltoid [34], the mid-forearm which is halfway from the ventral midline to the medial of FDS and FDP [38], the muscle 30% proximal between the medial malleolus of the fibula and the medial condyle of the tibia of gastrocnemius [33, 36, 39] and 20% of the distance from the head of the fibula to the tip of the lateral malleolus of TA [40, 44], BB was found at the distal third (i.e., 66%) of the total humeral length between the coracoid process of the scapula and the crease of the cubital fossa on the radial side or. at two-thirds of the position from the acromion to the crease of the elbow [33, 36], vastus lateralis and vastus intermedius was defined between the anterior superior iliac spine and the proximal end of the patella [37].
Quality assessment
Of the 13 included studies, 12 were of high quality (scores 6–9), while 1 was of low quality (score 4), as summarized in Table 3. The main reasons for point deductions included inadequate or missing descriptions of assessor blinding [32, 34,35,36,37, 39,40,41,42,43,44], and information reporting during reproducibility procedures [32, 34, 35, 39, 41, 43], as well as inappropriate minimization of contact pressure during ultrasound scanning [16, 31,32,33,34,35,36, 38,39,40,41,42, 44, 47].
Table 3. Methodological quality of the included studies [33,34,35,36,37,38,39,40,41,42,43,44]Reliability of ultrasound-based measurements
As summarized in Table 4, ultrasound demonstrated excellent intra- and inter-rater reliability (ICC >0.90) in assessing MT of the MG [32, 42], and moderate-to-excellent intra- (ICC = 0.74–0.92 [40]) and inter-rater (ICC = 0.69–0.96 [43]) reliability in measuring the MT of TA. Additionally, good-to-excellent inter-rater reliability was also observed in assessing MT of the deltoid (ICC = 0.84–0.93) [34], supraspinatus (ICC >0.98) [35], and abdominal muscles (ICC >0.92) [41].
Table 4. Reliability of muscle architectural measurements obtained from ultrasound [33,34,35,36,37,38,39,40,41, 43, 44]
Regarding PA, ultrasound exhibited moderate-to-excellent intra-rater (ICC = 0.69–0.99) and inter-rater (ICC = 0.70–0.98) reliability in MG assessment [39, 42]. Similarly, good-to-excellent intra-rater (ICC = 0.92/0.99 [40]) and inter-rater (ICC = 0.81–0.93 [18]) reliability were observed in TA.
For CSA, ultrasound also presented good-to-excellent intra-rater reliability in measuring CSA of the FDS (ICC = 0.82) [39], BB (ICC = 0.95) [33], and MG (ICC = 0.97) [33], as well as good-to-excellent inter-rater reliability in evaluating CSA of the FDS (ICC = 0.76/0.96) [39]. Furthermore, ultrasound demonstrated excellent intra- and inter-rater reliability for measuring MV in the TA, with all ICC values >0.9 ML assessment, it showed excellent intra- and inter-rater reliability (ICC >0.9) in the TA [43], along with good intra-rater reliability in the MG and BB, each with ICC values of 0.89 [33].
Table 5 summarizes the evidence for the reliability of ultrasound-based muscle measurements in post-stroke patients. Strong evidence supports moderate-to-excellent reliability for MT and PA. Moderate evidence indicates good-to-excellent reliability for CSA and ML and excellent reliability for MV.
Table 5. Level of evidence [33,34,35,36,37,38,39,40,41,42,43,44]