While tens of millions of Americans have tried to lose weight with the help of blockbuster medications, scientists say an alternative method is not only more effective, but also more sustainable long-term.
Researchers from New York University directly compared the effectiveness of semaglutide and tirzepatide, the active ingredients in weight-loss drugs Ozempic, Wegovy and Zepbound, with the more invasive yet permanent interventions of sleeve gastrectomy and gastric bypass for the first time in a new study.
For two years, they studied more than 14,000 people who had either taken the injectable GLP-1 drugs for at least six months or gotten surgery.
Over two years, surgery patients lost an average of 58 pounds, compared to just 12 pounds for those on medication, resulting in a massive 46-pound gap in total weight loss.
Bariatric surgery is a one-time procedure that delivers transformative, long-term results, while GLP-1 medications require expensive, lifelong monthly injections. Since most people eventually stop the medication and regain weight, the surgery is typically seen as the more effective option.
Dr Avery Brown, a surgical resident at NYU Langone Health and lead study author, said: ‘Clinical trials show weight loss between 15 percent to 21 percent for GLP-1s, but this study suggests that weight loss in the real world is considerably lower even for patients who have active prescriptions for an entire year.’
The sharp difference in results could be partly since as many as 70 percent of GLP-1 users stop taking their prescriptions for a variety of reasons, such as unmanageable side effects or cost. Surgery, meanwhile, is permanent and creates more sustained weight loss.
Despite the efficacy of surgery far outstripping that of medications, far fewer people opt for an operation every year compared to the number of people who get a prescription every year, about 280,000 and 8.4 million, respectively.

The number of people who choose surgery to lose weight is vastly outnumbered by those who receive prescriptions; about 280,000 operations versus 8.4 million prescriptions annually (stock)
Your browser does not support iframes.
Dr Brown said: ‘GLP-1 patients may need to adjust their expectations, adhere more closely to treatment or opt for metabolic and bariatric surgery to achieve desired results.’
A sleeve gastrectomy is a minimally invasive weight-loss surgery where about 80 percent of the stomach is surgically removed. This permanently reshapes the stomach into a narrow tube, or ‘sleeve,’ which significantly restricts food intake and reduces hunger hormones, promoting significant, lasting weight loss.
Gastric bypass is a procedure that surgically creates a small stomach pouch and reroutes a portion of the small intestine. The two-part approach works by both drastically restricting how much food a person can eat and by reducing the body’s ability to absorb calories and nutrients, leading to sustained weight loss.
Both procedures are typically highly successful. Patients undergoing sleeve gastrectomy typically lose around 50 to 70 percent of their excess body weight, with some losing up to 25 percent of their total body weight. After gastric bypass, patients typically lose 60 to 80 percent of their excess body weight.
GLP-1 drugs mimic a hormone that signals to the brain to stop eating and helps quell cravings. They also come with an array of side effects, from mild nausea to life-disrupting changes in bathroom habits.
Researchers began with a large pool of more than 140,000 patients who either took medications for at least six months (122,595 patients) or underwent weight-loss surgery (18,136 patients) between 2018 and 2024.
The medication group had higher rates of obesity and chronic obstructive pulmonary disease (COPD). Without accounting for these baseline differences, it would be impossible to determine whether the results were due to the treatment or to these other health factors.
The researchers used an advanced statistical technique called propensity score matching, which acts like a matchmaker, finding a ‘surgery twin’ for each ‘medication twin’ based on key characteristics such as age, starting weight and blood sugar, resulting in about 14,000 matched pairs.


Jenn Erskine, now 36 years old and from Florida, lost 370lbs after receiving weight loss surgery. She is shown left at 546lbs, her heaviest, and now at 175lbs
Because people sometimes stop taking their medication, the team looked at the results in two ways: one included everyone who started treatment and the other only included those who kept taking their shots consistently.
In the real-world analysis of over 7,000 patients per group, surgery led to significantly greater weight loss.
After two years, surgery patients lost an average of about 26 percent of their total body weight, compared to about five percent for patients who were prescribed the injectable medications – making surgery five times more effective than injectables.
Then, the researchers conducted a rigorous analysis focusing only on the 146 patients in each group who followed their treatment plan perfectly for two full years, meaning that medication patients took their shots continuously.
In this ideal scenario, the gap narrowed, but surgery was still three times more effective. The perfect-use medication group lost about eight percent of their body weight, while surgery patients lost about 25 percent.
Additionally, surgery was also better at improving long-term blood sugar control over the two-year period, an outcome that is particularly important for obese people who also have diabetes.
Dr Ann M Rogers, president of the American Society for Metabolic and Bariatric Surgery, which funded the research, said: ‘While both patient groups lose weight, metabolic and bariatric surgery is much more effective and durable.
‘Those who get insufficient weight loss with GLP-1s or have challenges complying with treatment due to side effects or costs, should consider bariatric surgery as an option or even in combination.’

Surgery works by physically changing the stomach and gut to limit food intake and hormones. The medications work by mimicking a hormone that reduces appetite in the brain
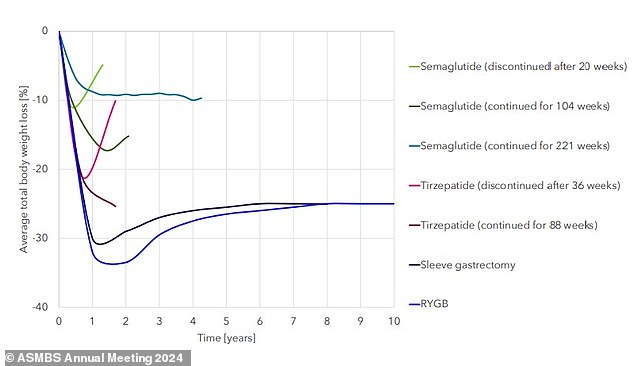
In 2024, researchers compared sustained weight loss across groups being treated for obesity. Bariatric surgery (sleeve, RYGB) led to the most significant initial weight loss as well as a loss of about 25 percent of their body weight up to a decade after surgery
Their results were presented at the American Society for Metabolic and Bariatric Surgery 2025 Annual Scientific Meeting in June.
Previous research has arrived at similar results.
In a study published in September, researchers in Pennsylvania tracked the health records of more than 30,000 obese people enrolled in a state insurance plan who were either prescribed an injectable drug or who underwent bariatric surgery. To ensure a fair comparison, researchers matched people by age and past health problems.
Surgery was significantly more effective. Over about two years, surgery patients lost an average of 28 percent of their body weight, compared to 10 percent for patients on the medications.
In another separate study in 2024, researchers from New York, Germany, and Austria conducted a major review comparing long-term outcomes of weight-loss surgery and the new injectable medications in roughly 20,000 patients.
Weight loss was significant and long-lasting. Patients lost about 30 percent of their body weight one year after surgery. They maintained 25 percent of their weight loss for up to ten years, demonstrating long-term results.
In people who took the injectable drugs, weight loss was substantial but plateaued. After about 17 to 18 months, the maximum loss was around 22.5 percent for tirzepatide (Mounjaro/Zepbound) and between 10 to 15 percent for semaglutide (Wegovy/Ozempic).
They also found that stopping the medication led to regaining about half the lost weight within one year.
While bariatric surgery involves a higher upfront cost and a more intense recovery, it is an investment that fundamentally changes the body’s physiology, allowing for lasting success.
The one-time procedure sets a patient on a definitive path to significant, sustained weight loss and overall health improvement, which may prove more cost-effective and impactful over a lifetime than managing a costly, indefinite monthly prescription for Wegovy or a similar drug.
