Definition of a post-ICU patient (GRIP consensus)
The GRIP consortium defined a post-ICU patient as:
” Any adult patient who has been admitted to an ICU for more than 48 h and is in the post-ICU recovery phase, which begins after the first ICU discharge and continues for up to one year, regardless of hospital length of stay, readmissions, or discharge destination (hospital ward, rehabilitation, home, or institution).”
The threshold of an ICU admission duration of more than 48 h was selected to identify patients at increased risk for post-ICU malnutrition and long-term complications [17]. Focusing on this population enables studies to assess the impact and outcomes of nutritional interventions more effectively in those who are most likely to benefit. Patients admitted for shorter durations, often for elective surgical procedures or brief monitoring, typically exhibit limited physiological distress [18]. Additionally, brief ICU stays do not provide sufficient time to warrant extended nutritional follow-up, and patients will likely not receive nutritional support (i.e., enteral (EN) or parenteral nutrition (PN)) in the ICU.
Importantly, the post-ICU phase is defined as beginning immediately after the first ICU discharge, irrespective of subsequent readmissions. This definition ensures continuity in capturing the non-linear nature of recovery and planning of nutritional care.
A recovery period of up to one year was selected based on evidence that the physiological, nutritional, and functional effects of critical illness can persist well beyond hospital discharge [19, 20]. This timeframe enables comprehensive monitoring of PICS manifestations and accounts for the diversity of recovery trajectories, ranging from rapid improvement to prolonged, or complicated recovery courses.
The definition deliberately includes patients with prolonged, recurrent, or complicated critical illness and encompasses all discharge destinations, whether to hospital wards, rehabilitation centres, long-term care institutions, or home. This broad scope reflects the heterogeneity of the post-ICU population, ensuring that research findings remain applicable across diverse healthcare settings [21, 22].
By establishing an inclusive and standardised definition, GRIP aims to align study designs, enhance comparability across research efforts, and support the development of nutritional strategies throughout the recovery continuum.
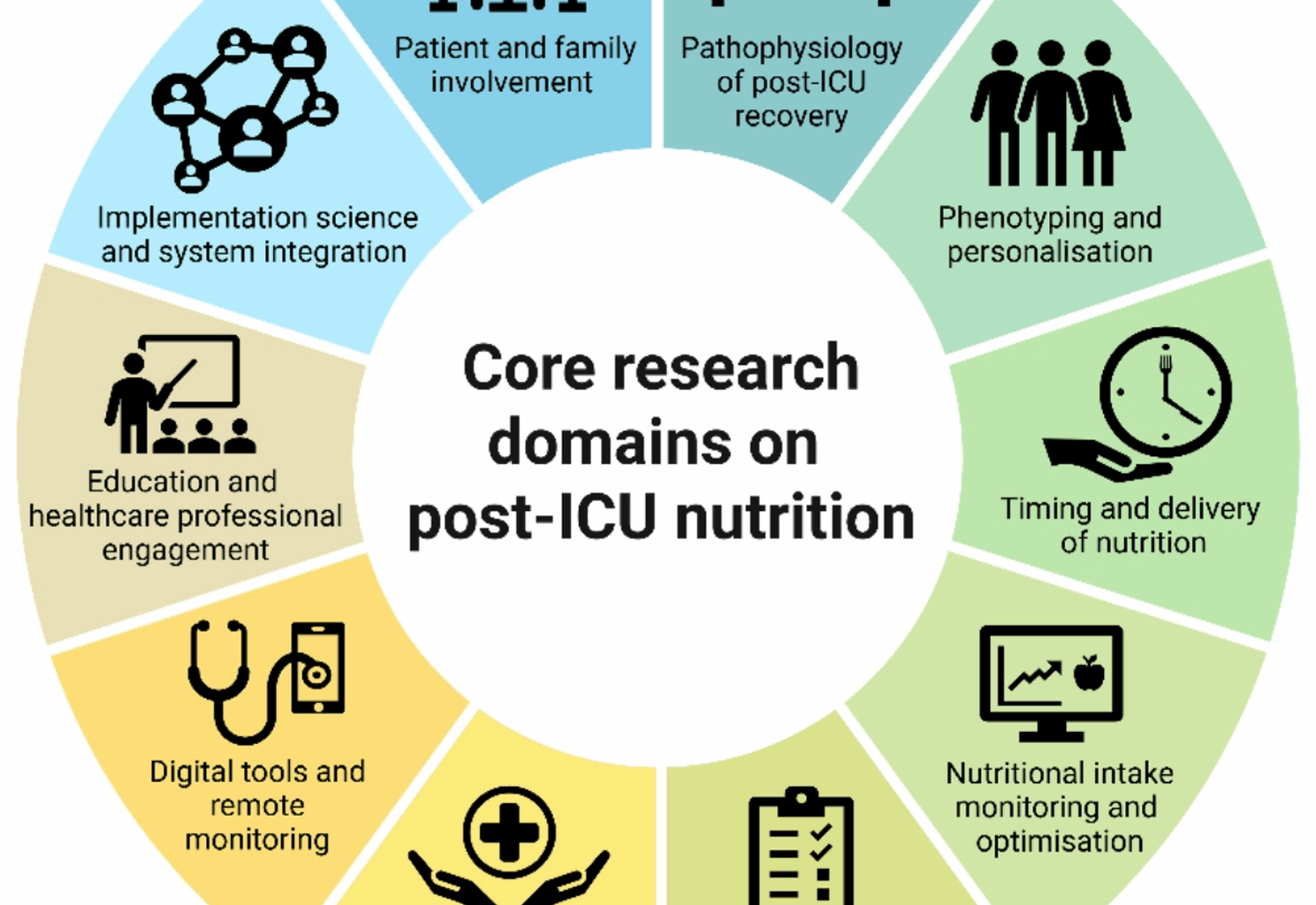
Identified Core Post-ICU Nutrition Research Domains by the GRIP Consortium. Created in https://BioRender.com
Core post-ICU nutrition research domainsPathophysiology of post-ICU recovery
Critical illness exerts profound physiological stress on multiple metabolic processes, with both immediate and long-lasting consequences, even following relatively short ICU stays [23, 24]. One of the hallmark responses is protein catabolism, characterised by muscle atrophy, mitochondrial dysfunction, insulin resistance, and impaired wound healing [25]. The long-term sequelae can include ICU-AW, which encompasses reduced muscle strength, critical illness-myopathy, polyneuropathy, and endocrine disruption [26,27,28]. These pathophysiological changes underlie the development of PICS.
Recovery is a multifaceted process that extends beyond hospital discharge [29]. Modest functional gains may support and accelerate the improvement of metabolic health, ultimately enhancing the body’s natural recovery trajectory [30]. A recent review identified weight change as the most prevalent nutritional outcome tracked in patients post critical illness, highlighting the ongoing catabolic stress that persists into the recovery phase [31].
The pathophysiology of post-ICU recovery reflects a complex interplay between acute critical illness and individual patient vulnerabilities. Effectively addressing this complexity demands targeted, individualised strategies that extend beyond the ICU and hospital stay, supporting long-term recovery across all phases of care.
Phenotyping and personalisation
Given the heterogeneity of patients post-ICU, nutritional interventions should shift from a one-size-fits-all approach to a more tailored treatment strategy [32]. These patients face various physiological, functional, and psychological barriers during the acute phase of critical illness, which persist during the recovery phase on the ward and in the long-term recovery after hospital discharge (Fig. 2) [16, 33, 34]. These challenges complicate the transition to full oral intake and increase the risk of underfeeding [22].
Besides these challenges, nutritional therapy could be tailored to the patient’s metabolic rate, body composition, and clinical phenotype [35, 36]. Recent studies emphasise the importance of body composition assessments in determining individualised energy and protein requirements, recognising that factors, such as sex-related differences in lean body mass, influence nutritional needs [37]. Additionally, anabolic resistance in critically ill patients impairs the muscle protein synthesis response to nutrition provision, potentially limiting the effectiveness of nutritional interventions during ICU stay and the recovery period [38]. Emerging research highlights the utility of indirect calorimetry (IC), bio-electrical impedance analysis (BIA), and potential biomarkers to guide personalised nutritional strategies [32, 37, 39,40,41,42,43]. However, implementing these approaches in the post-ICU phase remains challenging, due to logistical constraints, limited clinical evidence and the lack of well-established benefits. Not only is nutrition in the post-ICU phase important, but patients’ pre-existing dietary regimes should also be carefully considered. Accommodating for individual dietary regimes is essential as limited or unsuitable nutritional options can also lead to inadequate nutrition. Nutrition such as gluten-free, lactose-free, vegetarian and vegan, can be associated with potential deficiencies in vitamins, trace elements, and calcium. Since EN and PN are typically not tailored to these specific diets, unintentional exposure to gluten or lactose during and post-ICU may lead to intolerances or allergic reactions [44].
Beyond medical and physiological heterogeneity, it is increasingly recognised that social determinants of health, such as pre-existing malnutrition, poverty, and social deprivation, strongly influence recovery after critical illness [45, 46]. These factors impact access to adequate nutrition, rehabilitation, and long-term support systems, and therefore must be considered when developing personalised post-ICU strategies.
While different elements are only briefly acknowledged in the present position paper, they represent important research priorities that will be further explored in subsequent research dedicated to this domain.
Challenges and Opportunities Regarding the Continuum of Post-ICU Nutritional Care. ICU: intensive care unit; PICS: post-intensive care syndrome. Created in https://BioRender.com.
Timing and delivery of nutrition
The timing and delivery of nutrition play a crucial role in aligning with patients’ biological rhythms and maximising anabolic potential. Hospital routines frequently interfere with this process, for instance, morphine administration prior to meals, and a lack of protected mealtimes. Dinner, which is typically the most protein-rich meal, is also the most frequently wasted [47]. A systems-level redesign of hospital food provision is needed to support culturally sensitive nutrition delivery synchronised with physiological recovery phases, and individual preferences and habits. The concept of chrono-nutrition, first introduced in 1986, refers to a dietary approach that emphasises alignment with circadian fluctuations in metabolism [48, 49]. Complementary domains, such as nutrigenetics and microRNA-mediated epigenetic modulation, represent emerging areas of interest in personalised nutrition [50, 51].
In addition to timing and genetic influence, reinitiation, and escalation are integral parts of post-ICU protocols, which will continue to evolve based on emerging evidence. Diminished appetite, changes in taste, nausea, and dysphagia are commonly reported barriers faced by patients during hospitalisation and beyond [21]. These patient-related barriers are compounded by organisational and logistical constraints that hinder the timely and effective delivery of nutrition.
Addressing both patient and organisational barriers is crucial for developing comprehensive, future oriented protocols. As the majority of patients are discharged from the hospital relying solely on oral nutrition despite ongoing physical impairments, it is vital to conduct research throughout the recovery phase, particularly after hospital discharge [21].
Nutritional intake monitoring and optimisation
Adequate and effective nutritional therapy for patients post-ICU should be built upon the principles established during their ICU stay. Current guidelines, such as those from the European Society for Clinical Nutrition and Metabolism (ESPEN) and the American Society for Parenteral and Enteral Nutrition (ASPEN) [52, 53], lack guidelines regarding post-ICU follow-up.
In the post-ICU phase, underfeeding remains a significant concern. However, studies examining adequate protein and energy targets in the post-ICU phase are scarce [21]. Energy targets during the post-ICU phase are recommended at 125% of measured resting energy expenditure, or 30 kcal/kg/day if IC is unavailable, with protein targets set at 1.5–2 g/kg/day. Even higher targets are recommended during the post-hospitalisation phase [54]. Several studies have shown that energy and protein intake were lower than estimated or measured compared to requirements during the post-ICU hospitalisation period [21]. Additionally, it is observed that patients transitioning from the ICU to the general ward who rely solely on oral intake are at the highest risk of experiencing a nutritional deficit [22, 55,56,57,58]. Few randomised controlled trials (RCTs) focusing on the post-ICU phase exist regarding protein and energy intake, however demonstrating no impact on clinical outcomes including duration of hospital stay, ventilator-free time, and bloodstream infection rate [59].
Even less is known about nutrition after hospital discharge. A review of studies that provided follow-up within 12 months of hospital discharge recorded energy and protein targets and intake [31]. The majority of patients did not meet energy and protein targets that were set. After a 12-month follow-up period, most patients relied solely on oral nutrition or a combination of oral and oral nutritional supplements (ONS).
Monitoring of nutritional intake is often a hurdle during the post-ICU phase and can be challenged by a lack of registration by ward staff, difficulties in registering in electronic systems, and the involvement of family [22]. To enable the monitoring of oral intake, simplified tools, such as digital food charts and scoring systems that involve patients and caregivers, are needed. However, the link between post-ICU nutrition and long-term outcomes remains insufficiently understood, underscoring the need for targeted research and the adaptation of guidelines.
Nutrition interventions and effectiveness
Relying solely on oral nutrition frequently results in inadequate intake among patients post-ICU, which can be countered by providing supplemental EN or PN [60]. Studies have investigated the absorption rate of food, oral supplements, and EN in this population. These studies found that while gastric emptying is delayed in critical ill patients, it tends to recover rapidly after discharge from the ICU [34, 61].
A variety of nutritional approaches should be compared to oral intake that fails to meet targets, including ONS, EN and PN. Before making the transition to artificial nutrition, providing in-between energy- and protein-enriched meals can also enhance nutritional adequacy [62, 63]. In addition to optimising delivery routes and timing, specific nutritional interventions warrant further investigation in the post-ICU setting. Interventions of particular interest include immunonutrition blends, omega-3 fatty acids, ketone supplementation, and anabolic agents such as β-hydroxy-β-methylbutyrate (HMB). While the evidence base in post-ICU patients is currently limited, these interventions hold potential to modulate metabolic pathways relevant to recovery [64,65,66,67,68,69].
Next to the administration route and timing, dosing precision is also evolving. In recent years, energy targets have shifted from predictive equations to IC-based approaches. However, protein targets are still primarily based on weight-based formulas, and no individualised approach is currently available.
Daily assessment of nutritional energy and protein adequacy, along with the evaluation of the nutritional dosing approach, can serve as the basis for evaluating the effectiveness of nutritional interventions and guide real-time adjustments to nutritional therapy.
Studies conducted in patients post-ICU have addressed the difficulties associated with recording oral intake. Technologies, such as wearables, artificial intelligence, and mobile apps, could help patients and staff accurately record oral intake and activity.
Long-term functional and health-related quality of life outcomes
Assessing the impact of nutrition on long-term recovery outcomes, including physical function and HRQoL, is crucial. This assessment requires pragmatic, patient-centred tools, wearable activity monitors, and remote follow-up systems to track progress and outcomes beyond discharge [70].
Nutrition should not be viewed in isolation but as a critical component of integrated rehabilitation. Emerging concepts such as the NEXIS trial design [71], which combines exercise and nutritional interventions, underline the potential of multidomain approaches to improve long-term outcomes. Similarly, validated multidomain screening tools, such as the PICUPS instrument [72, 73], allow assessment of nutrition within the broader context of PICS.
To support effective follow-up strategies, structured rehabilitation pathways are needed. These could differentiate between early post-ICU care and long-term post-discharge recovery, and incorporate regular assessments, consultations, and outcome monitoring [74]. Although similar rehabilitation pathways exist for other patient populations, patients post critical illness remain underserved in this regard [75, 76]. Furthermore, while a core-outcome set has been defined for the evaluation of metabolic and nutritional interventions in critically ill patients [77], no predefined set of outcomes exists for the post-ICU phase. The establishment of these sets would guide future research, enhance comparability of results across studies, and facilitate more robust conclusions.
Digital tools and remote monitoring
Technology plays a pivotal role in advancing post-ICU nutritional management by enabling continuous monitoring, improved data sharing, and patient-centred care. Electronic health records are central to this, supporting the documentation and longitudinal assessment of nutritional status across the care continuum. When integrated with nutrition-specific software, these health records allow real-time tracking of key nutritional parameters and outcomes, facilitating individualised care adjustments, and supporting continuity from ICU to outpatient settings.
Telemedicine, initially scaled during the COVID-19 pandemic, has become a valuable tool for remote nutrition monitoring. Virtual consultations offer a practical solution when in-person visits are not feasible, allowing clinicians to detect early signs of nutritional decline, adjust interventions promptly, and enhance patient and caregiver engagement [78, 79]. This support is particularly important during the transition from the ward to home or rehabilitation when patients are vulnerable to setbacks in nutritional recovery. Looking forward, wearable technologies hold the potential to decentralise nutritional monitoring. Emerging devices could enable at-home measurement of the patient’s metabolic rate, muscle strength, glucose monitoring, and body composition, offering clinicians a clearer view of recovery while reducing the need for in-hospital assessments [80]. Artificial intelligence-driven applications may also support patient self-monitoring by facilitating dietary tracking, HRQoL assessments, and nutritional goal setting [81].
To maximise the value of digital tools, the data gathered through digital tools must inform clinical decision-making and quality improvement. Embedded feedback systems, such as electronic health records and clinical dashboards, can alert clinicians to deviations from nutritional goals, identify patients at risk, and track recovery trajectories [82]. Combining this data with patient-reported outcomes enables iterative refinement of care pathways and protocols [83].
Post-ICU clinics represent a key platform for applying these tools in practice. They offer opportunities for ongoing nutritional reassessment, care planning, and education for patients and their families. However, their structure varies widely in terms of eligibility criteria for the patients, involved professionals, type of care provided, timing and frequency of appointments, and outcome measurement tools [84,85,86]. To address this, pilot programs should test unified protocols and technologies in select settings. These pilots can assess feasibility, streamline workflows, and gather early feedback to inform broader implementation. Embedding dietitians in these initiatives ensures high-quality, individualised nutritional care.
Education and healthcare professional engagement
A sustainable post-ICU nutritional care framework depends on the engagement and continuous education of healthcare professionals across all care settings. Persistent knowledge gaps and unclear roles contribute to inconsistent practices and poor outcomes for post-ICU patients.
To address these challenges, nutrition education should be integrated throughout professional development. Interdisciplinary training that brings together physicians, nurses, dietitians, and pharmacists fosters collaboration and enhances role clarity [86,87,88]. Certification programs in clinical nutrition can help standardise competencies, ensuring consistent practice across institutions.
Continuing education must keep pace with evolving evidence, including new assessment technologies, recognition of post-ICU malnutrition, and protocols for post-discharge nutritional follow-up [89]. Crucially, these educational efforts must be tailored not only to clinical complexity but also to clinical variability, ensuring relevance for both high-resource and resource-limited healthcare environments [87, 90]. Digital education models offer scalable solutions. Online learning platforms, self-paced modules, virtual simulations, and tele-mentoring programs allow flexibility and provide important opportunities for lifelong learning [91, 92].
Post-ICU nutritional care engagement also relies on shared responsibility. Embedding dietitians into ward rounds and discharge planning can bridge care transitions, while stronger collaboration between ICU teams, general wards, rehabilitation units, and community-based providers supports continuity of care. This integrated, team-based approach reinforces nutrition as a critical thread throughout the recovery journey, ultimately enhancing patient outcomes [93,94,95,96].
Training in quality improvement methodologies, audit tools, and implementation science equips professionals to evaluate adherence to protocols, monitor outcomes, and adapt strategies based on local data [97]. Digital tools, such as electronic health records, mobile apps, and remote monitoring, can support real-time evaluation and facilitate continuous learning.
Ultimately, educational initiatives must be inclusive, interdisciplinary, and adaptable to local needs and contexts. By empowering healthcare professionals through accessible, relevant training and promoting collaborative practice models, nutrition can be fully embedded as a cornerstone of post-ICU recovery.
Implementation science and health systems
Despite growing awareness of its importance, post-ICU nutritional care remains inconsistently implemented, often hindered by systemic barriers, including unclear team responsibilities, low staff engagement, and variable discharge practices. These challenges underline the urgent need for structured, system-wide solutions to embed nutrition into the standard of post-ICU care.
These systemic issues become even more pronounced during the transition from ICU to the ward, rehabilitation, and ultimately home, which are vulnerable phases where nutritional strategies are often interrupted [22, 55, 56]. To support continuity, flexible, context-sensitive strategies that span the entire recovery process are essential. Discharge planning must consider local staffing levels, outpatient resources, and the patient’s specific risks and needs.
A coordinated, global approach is necessary to standardise care and reduce variability across settings. This strategy involves the development of protocols based on quality assurance and benchmarking practices [98, 99]. Initiatives like NutritionDay, launched in 2007 and now extended to ICUs and nursing homes worldwide, demonstrate the feasibility and power of large-scale data collection, as well as its utility in identifying care gaps, comparing outcomes internationally, and informing improvements in training, protocols, and service delivery [100].
To ensure consistent quality, certification and accreditation frameworks, aligned with bodies, such as ESPEN, ASPEN and Australasian Society of Parenteral and Enteral Nutrition (AuSPEN), can guide the standardisation of post-ICU nutrition care. These frameworks should define minimum care levels, core competencies, and structured care pathways further to promote consistency across healthcare systems [101].
Measuring implementation success requires a robust, multidimensional evaluation. This assessment includes identifying key performance indicators relevant to both inpatient and outpatient settings, such as nutritional adequacy, readmission rates, functional recovery, and patient-reported HRQoL [77, 102, 103]. These clinical outcomes should be complemented by qualitative feedback from patients, families, and healthcare providers, offering valuable insights into practical barriers and opportunities for improvement [104].
Sustaining research and quality improvement efforts requires strong multi-sector partnerships [105]. While investigator-initiated studies can drive innovation, coordinated support from governments, academic institutions, industry, and advocacy organisations is essential to fund, scale, and evaluate post-ICU nutrition initiatives globally [106, 107].
The provision of nutrition to inpatients demonstrated improvements in patient outcomes along with cost savings. It reduces the overall healthcare economic burden and emphasises the role of the governments in ensuring funding to facilitate effective nutritional interventions in hospitals [108].
Patient and family involvement
Patient and family engagement is central to successful post-ICU nutritional care. Recognising that recovery extends well beyond ICU discharge, nutritional strategies must be co-developed with patients and caregivers, communicated clearly, and tailored to reflect the beliefs, preferences, and daily realities.
Engaging patients and caregivers in setting realistic, personal goals helps ensure that these nutrition plans are feasible and sustainable in their home environments [109, 110]. Early engagement fosters trust and supports long-term self-management.
Education is a key enabler of this engagement, providing clear explanations of nutritional goals, the risks of undernutrition, and practical strategies for recovery. Accessible tools, such as brochures, informative videos, and mobile applications, can be helpful in this guidance [111]. These resources can reinforce the link between nutrition, physical rehabilitation, and independence [112, 113].
Cultural sensitivity could further enhance engagement, by accommodating religious practices, traditional dietary habits, personal preferences, food accessibility, and affordability [114]. For example, protein intake goals may need to be adjusted to align with dietary habits, local food availability, or the increasing shift from animal-based to plant-based protein sources.
Sustained engagement relies on proactive communication and coordinated care [115]. Regular check-ins, whether through in-person clinic visits, telehealth services, or phone calls, enable timely adjustments, and provide valuable feedback. Involving dietitians early in discharge planning supports continuity and helps bridge knowledge gaps between inpatient and community care.
Empowering patients and caregivers through education, collaboration, and culturally responsive care enhances the effectiveness of interventions. By building trust, ensuring clear communication, and fostering community support, healthcare systems can significantly improve the long-term outcomes of patients post-ICU.