Patient selection and groups
This retrospective study was conducted following approval from the local ethics committee. A total of 93 patients with isolated medial meniscus tears, with tear types recorded, and treated using either the outside-in (OI) or all-inside (AI) technique, were included in the study. Patients were recruited from two different orthopedic clinics.
Inclusion criteria consisted of: Age ≥ 18 years, Isolated medial meniscus tear located in anatomical zone-3 or zone-4 [6, 8, 22], A history of knee pain lasting no longer than three months, Positive meniscus tear signs on physical examination (McMurray test, joint line tenderness, or Apley test), Magnetic resonance imaging (MRI) confirmation of a medial meniscus tear, and surgical repair using either the OI or AI technique.
Exclusion criteria included patients who had previously undergone a surgical procedure on the affected knee, as well as those with a concurrent lateral meniscus tear, medial meniscus posterior root tear, or varus malalignment, which is defined as hip-knee angle < 175. Additionally, patients with grade 3 or 4 cartilage damage, multiple ligament injuries, anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL) injuries, and those younger than 18 years or older than 65 years were excluded from the study. All meniscal repairs were performed by two experienced orthopedic surgeons, each exclusively using one technique—outside-in (first author) or all-inside (third author)—both with over five years of experience in arthroscopic knee surgery, between 2020 and 2023, with a minimum follow-up of six months. Patients were divided into two groups (OI and AI) based on the technique used for meniscus repair (Fig. 1).
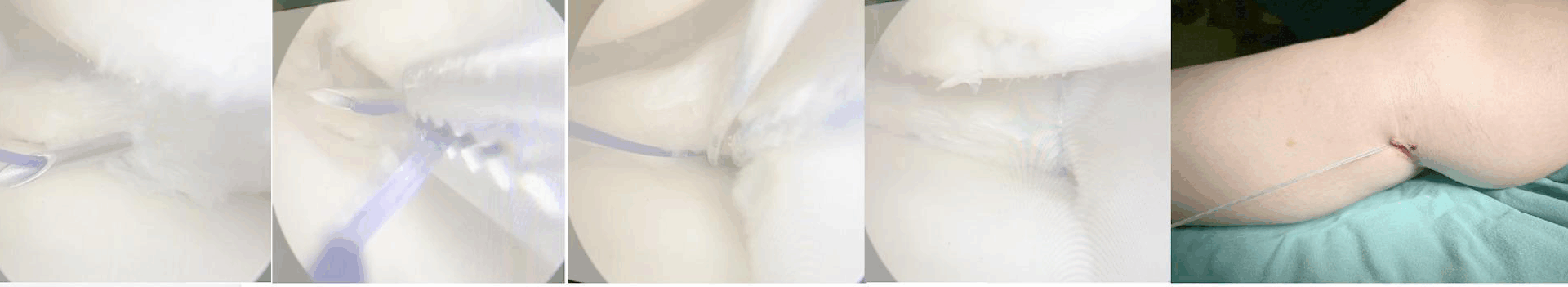
Illustrates the outside-in suture shuttle repair technique, utilizing a 16-gauge intravenous cannula and a small posteromedial knee incision
Surgical techniques
OI meniscal repair was performed in 63 cases, while AI meniscal repair was performed in 30 cases. A 16-gauge intravenous (IV) cannula and 2.0 non-absorbable Prolene sutures were prepared. A standard 16-gauge IV cannula needle was inserted through the skin into the medial compartment of the knee joint using transillumination for guidance. Once the needle penetrated the capsule and passed through the meniscal tear—according to the planned suture configuration (vertical or horizontal mattress)—the Prolene sutures were retrieved to the outer surface of the knee via the anteromedial portal.
The Fiber-Wire knot was secured to the loop of the 2.0 Prolene suture and advanced to the posterior aspect of the knee. Subsequently, a small incision and tunnel were created on the capsule. A 16-gauge needle was then inserted through the pre-formed tunnel and directed appropriately toward the meniscal tear. The 2.0 Prolene suture within the needle was retrieved through the anteromedial portal to the anterior surface of the knee. The Prolene loop was tied to the anterior end of the 2.0 Fiber-Wire and transported back to the posteromedial aspect of the knee (Fig. 1).
In the final step, the Fiber-Wire was securely tied and fixed to the outer surface of the capsule [5, 13].The AI meniscus repair technique was performed using a preloaded meniscal repair device (FasT-Fix), which was inserted through the working portal. The first suture anchor was deployed inside the joint to secure the meniscal tissue, followed by the placement of the second anchor at the desired location. Finally, the pre-tied sliding knot was tightened to approximate the tear edges [1].
Data collection
Additionally, demographic characteristics, including age, sex, history of previous knee surgeries, and tear zone location, were recorded. Postoperative complications such as deep vein thrombosis, saphenous nerve palsy, septic arthritis, or medial knee pain requiring second-look surgery were also documented.
At a minimum follow-up of six months postoperatively, patients completed a subjective questionnaire to assess clinical outcomes at the last follow-up. The evaluation included the Knee Injury and Osteoarthritis Outcome Score (KOOS), the Tegner-Lysholm Knee Scoring Scale (TLKS), and the International Knee Documentation Committee (IKDC) score. Clinical outcomes were analyzed using the Minimal Clinically Important Difference (MCID) values for each measure [15].
Rehabilitation
During the first three weeks, knee flexion was restricted to 90°, with full extension being the primary goal. Patient mobilized with knee brace and double crutches. Weight-bearing was not permitted during this period. Early rehabilitation exercises included straight leg raises, hip abduction, and ankle pumps. From week 3 to week 6, partial weight-bearing was gradually introduced, and range of motion (ROM) and stretching exercises were performed to achieve at least 120° of knee flexion. The knee brace lock was removed as stability improved. After week 6, the use of the brace and crutches was discontinued. Stationary cycling was initiated to facilitate the transition to functional activities. Strengthening exercises were progressively advanced to improve muscle endurance and joint stability. Patients were advised to return to unrestricted sports activities between 4 and 6 months postoperatively, depending on individual recovery and adherence to the rehabilitation protocol.
Statistical analysis
Data analysis was performed using ‘’IBM SPSS Statistics 26’’. Categorical independent variables were presented as frequencies and percentages with cross-tabulations. Their distributions were compared using ‘’Chi-Square Test’’ or ‘’Fisher’s Exact Test’’ method. The suitability of continuous variables for normal distribution was investigated using graphical examination (Q-Q Plot), normality tests (Shapiro-Wilk) and sample size. Independent group comparisons of variables conforming to normal distribution were made with the ‘’t test’’ and presented with mean and standard deviation. For variables not conforming to normal distribution, the ‘’Mann Whitney’’ test was used and presented with median (min-max). For the difference in measurements taken before and after surgery, ANCOVA analysis was performed for repeated measurements in the comparisons between the groups and correction was made according to age, crude and estimated marginal means were used to assess the patient reported outcomes pre- and post-operatively. Adjusted means are presented. Effect sizes are presented as partial eta squared. In all statistical comparison tests, type-1 error margin was determined as α:0.05 and tested as two-tailed. The MCID was calculated using a distribution-based approach, employing the 0.5 standard deviation (SD) method for each outcome measure (IKDC, KOOS, TLKS). Preoperative SD values were used to determine MCID thresholds for both the outside-in (OI) and all-inside (AI) groups [25].