Rauch F, Glorieux FH. Osteogenesis imperfecta. Lancet. 2004;363(9418):1377–85.
Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet. 1979;16(2):101–16.
Forlino A, Cabral WA, Barnes AM, Marini JC. New perspectives on osteogenesis imperfecta. Nat Rev Endocrinol. 2011;7(9):540–57.
Van Dijk FS, Sillence DO. Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet A. 2014;164A(6):1470–81.
Swezey T, Reeve BB, Hart TS, et al. Incorporating the patient perspective in the study of rare bone disease: insights from the osteogenesis imperfecta community. Osteoporos Int. 2019;30(2):507–11.
Rodriguez Celin M, Kruger KM, Caudill A, et al. A multicenter study to evaluate pain characteristics in osteogenesis imperfecta. Am J Med Genet A. 2023;191(1):160–72.
Shepherd WS, Wiese AD, Cho HE, et al. Psychosocial outcomes of pain and pain management in adults with osteogenesis imperfecta: a qualitative study. J Clin Psychol Med Settings. 2024;31(3):614–27.
Widmann RF, Laplaza FJ, Bitan FD, Brooks CE, Root L. Quality of life in osteogenesis imperfecta. Int Orthop. 2002;26(1):3–6.
Gooijer K, Harsevoort AGJ, van Dijk Fs, Withaar HR, Janus GJM, Franken AAM. A baseline measurement of quality of life in 322 adults with osteogenesis imperfecta. JBMR Plus. 2020;4(12):e10416.
Tosi LL, Oetgen ME, Floor MK, et al. Initial report of the osteogenesis imperfecta adult natural history initiative. Orphanet J Rare Dis. 2015;10:146.
van Welzenis T, Westerheim I, Hart T, et al. The IMPACT survey: the humanistic impact of osteogenesis imperfecta in adults. BMC Public Health. 2024;24(1):3318.
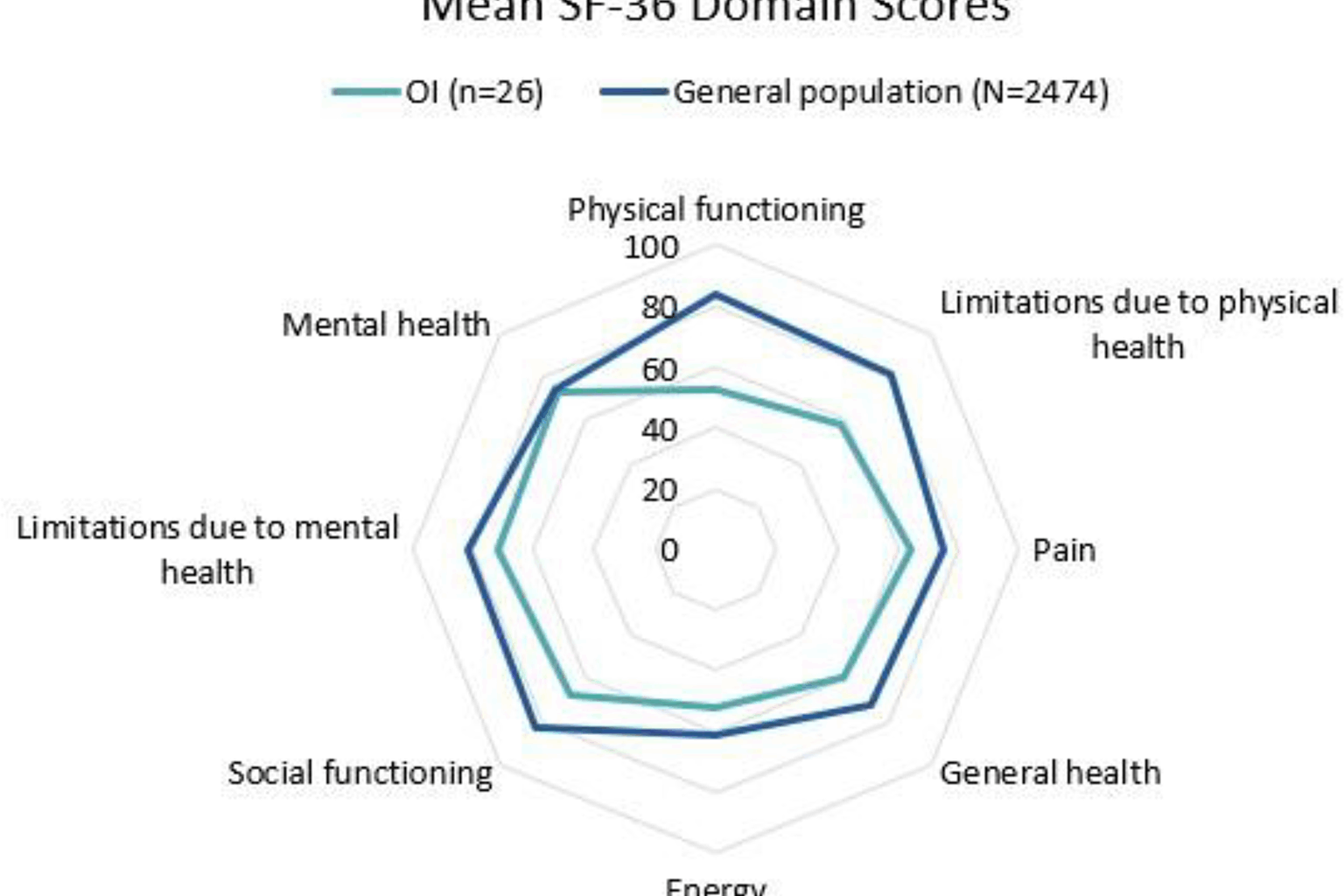
Fagereng E, Htwe S, McDonald S, Derocher C, et al. Mental health conditions, physical functioning, and health-related quality of life in adults with a skeletal dysplasia: a cross-sectional multinational study. Orphanet J Rare Dis. 2025;20(1):116.
Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med. 2001;33(5):350-7.
Yonko EA, Emanuel JS, Carter EM, Raggio CL. Quality of life in adults with achondroplasia in the United States. Am J Med Genet A. 2021;185(3):695–701.
Johansen H, Andersen I, Naess EE, Hagen KB. Health of adults with short stature: a comparison with the normal population and one well-known chronic disease (rheumatoid arthritis). Orphanet J Rare Dis. 2007;2:10.
Wright MJ, Thompson S, Shakespear TW. The restricted growth experience, quality of life, and barriers to participation. In: platform presentation at the International Skeletal Dysplasia Society. Albi, France; 2007.
Mahomed NN, Spellman M, Goldberg MJ. Functional health status of adults with achondroplasia. Am J Med Genet. 1997;78:30–35.
Matsushita M, Kitoh H, Mishima K, Yamashita S, Haga N, Fujiwara S, … Ishiguro N. Physical, mental, and social problems of adolescent and adult patients with achondroplasia. Calcif Tissue Int. 2019;104:364–72.
Hunter AGW. Some psychosocial aspects of nonlethal chondrodysplasias: I. Assessment using a life-styles questionnaire. Am J Med Genet. 1998;78:9–12.
Hunter AGW. Some psychosocial aspects of nonlethal chondrodysplasias: II. Depression and anxiety. Am J Med Genet. 1998;78:9–12.
Alves I, Fernandes O, Castro MA, Tavares S. Physical activity and psychosocial outcomes in adults with achondroplasia: an exploratory study. Int J Environ Res Public Health. 2024, Aug, 31;21(9):1160. https://doi.org/10.3390/ijerph21091160.
Matsushita M, Mishima K, Kamiya Y, Haga N, Fujiwara S, Ozono K, Kubota T, Kitaoka T, Imagama S, Kitoh H. Health-related quality of life in adult patients with multiple epiphyseal dysplasia and spondyloepiphyseal dysplasia. Prog Rehabil Med. 2021, Dec, 7;6:20210048.
Majoor BCJ, Andela CD, Quispel CR, Rotman M, Dijkstra PDS, Hamdy NAT, Kaptein AA, Appelman-Dijkstra NM. Illness perceptions are associated with quality of life in patients with fibrous dysplasia. Calcif Tissue Int. 2018, Jan;102(1):23–31.
Hays RD, Spritzer KL, Schalet BD, Cella D. PROMIS®-29 v2. 0 profile physical and mental health summary scores. Qual Life Res. 2018;27(7):1885–91.
PROMIS®. 2023. https://www.healthmeasures.net/explore-measurement-systems/promis. Accessed 28 Aug 2025.
Kumban W, Kanlayanaphotporn R, Khutok K. Comparative responsiveness of the PROMIS-29 and SF-36 instruments in individuals with chronic musculoskeletal pain. J Orthop Sci. 2025, Jul;30(4):704–10.
Chen CX, Kroenke K, Stump T, Kean J, Krebs EE, Bair MJ, et al. Comparative responsiveness of the PROMIS pain interference short forms with legacy pain measures: results from three randomized clinical trials. J Pain. 2019, Jun;20(6):664e75.
Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524–32.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–97.
Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–73.
Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: a review of its history, issues, progress, and documentation. J Rheumatol. 2003;30(1):167–78.
Duckworth AL, Peterson C, Matthews MD, Kelly DR. Grit: perseverance and passion for long-term goals. J Pers Soc Psychol. 2007;92(6):1087–101.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–81.
Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95:103–208.
Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L. The pain catastrophizing scale: further psychometric evaluation with adult samples. J Behav Med. 2000;23(4):351–65.
Krishnan E, Sokka T, Häkkinen A, Hubert H, Hannonen P. Normative values for the Health Assessment Questionnaire Disability Index: benchmarking disability in the general population. Arthritis Rheum. 2004;50(3):953–60.
Lucas JW, Connor EM, Bose J. Back, lower limb, and upper limb pain among U.S. adults, 2019. NCHS Data Brief. 2021;415:1–8.
Carvalho PAF, Regis TS, Faiçal AVB, Rmrds L, Terse-Ramos R, Acosta AX. Functional status of individuals with osteogenesis imperfecta: data from a reference center. J Pediatr (rio J). 2023;99(1):94–98.
Hinz A, Klein AM, Brähler E, et al. Psychometric evaluation of the generalized anxiety disorder screener GAD-7, based on a large German general population sample. J Affect Disord. 2017;210:338–44.
Ware J, Snoww K, Ma K, Bg G. SF36 health survey: manual and interpretation guide. Lincoln, RI: Quality Metric, Inc; 1993. 1993. p. 30.
Farivar SS, Cunningham WE, Hays RD. Correlated physical and mental health summary scores for the SF-36 and SF-12 health survey, V.I. Health Qual Life Outcomes. 2007;5:54.
Cella D, Choi SW, Condon DM, Schalet B, Hays RD, Rothrock NE, et al. PROMIS(®) adult health profiles: efficient short-form measures of seven health domains. Value Health. 2019;22(5):537–44.
Murali CN, Slater B, Musaad S, et al. Health-related quality of life in adults with osteogenesis imperfecta. Clin Genet. 2021;99(6):772–79.
Schoser B, Bilder DA, Dimmock D, Gupta D, James ES, Prasad S. The humanistic burden of pompe disease: are there still unmet needs? A systematic review. BMC Neurol. 2017;17(1):202.