Study design
This study employed a mixed-model design, including a between-group factor (experimental group who underwent the fatigue protocol vs. control group who did not undergo the fatigue protocol) and a within-subject factor (pre-fatigue vs. post-fatigue assessments). Male participants with ACLR and DKV were recruited for both groups.
Participants
A total of 44 males ACLR with DKV participants, divided into two groups, the experimental group (N = 22) and the control group (N = 22), based on G-power with effect size f 0.60, α error 0.05, power 0.80, degree of freedom 6, and covariate 1, aged 25–35 years to ensure a homogeneous sample and minimize age-related confounding factors, who had undergone ACLR with autograft hamstring were the standard procedure performed by the clinic and surgeon involved in this study, and were active in sports both before and following surgery, were selected for this study. Female participants were not included due to availability at the study setting. Participants were purposively sampled based on their suitability for the study, with strict adherence to inclusion and exclusion criteria. Inclusion criteria: having DKV, male athletes aged 25–35 years, history of ACLR with hamstring autograft, at least 6 months post-surgery, no history of other knee injuries, normal BMI (18–25), and voluntary participation and informed consent. Exclusion criteria: previous surgeries on the lower extremities (excluding ACLR), injury occurring during the study, failure to complete one of the tests, and multi-ligament injuries or osteochondral damage.
Experimental protocol
To induce fatigue, the experimental group underwent a Short-Stretching Cycle Fatigue Protocol [24, 25] during the testing session. The protocol involved 10 sets of 10 repetitions of forward and backward jumps, with a 30-second rest interval between sets. The participant stood in a neutral position with feet shoulder-width apart, with hands placed on the iliac crest opposite the metal bar attached to the wall, which was positioned 10 cm away. A tape measure was placed beside the bar to ensure accuracy in recording maximum and reduced jump height. Our exercise regimen is tailored to elicit peripheral functional fatigue, a specific type of fatigue that contrasts with central and mental forms. Participants were verbally encouraged to exert maximum effort throughout the protocol.
Before starting the fatigue protocol, each participant’s maximum jump height was recorded by marking the highest point reached on the metal bar, considered as the participant’s peak jump (100% of their jump capacity). A sub-maximal jump was defined as 70% of their maximum jump height. The fatigue protocol was continued until the participant could no longer perform a jump beyond the sub-maximal threshold, signaling that the fatigue level had been reached, at which point the protocol was discontinued [24]. Following the fatigue protocol, the post-test assessments were immediately repeated to evaluate. The control group comprised ACLR participants with DKV who were assessed at the same time points as the experimental group, but did not perform the fatigue protocol.
Outcome measures
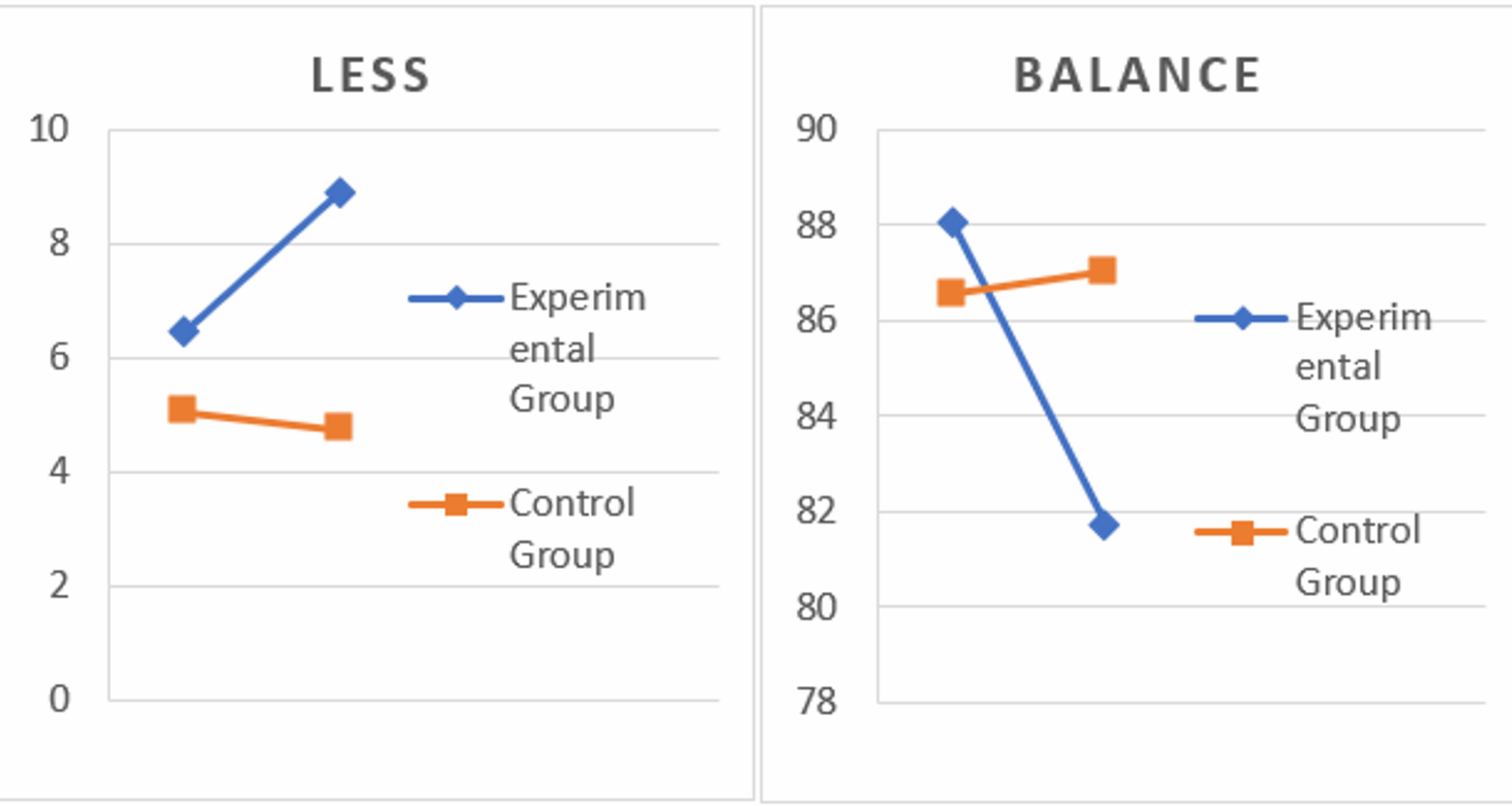
Primary outcome measures assessed lower-limb kinematics, jump-landing mechanics evaluated with LESS [26]. Dynamic balance, quantified through the Y-Balance test [27], was performed unilaterally on the involved limb. This test required maximal reach in anterior, posteromedial, and posterolateral directions while maintaining a single-leg stance. Proprioceptive acuity was measured via active joint repositioning tasks at 30° and 60° of knee flexion, with angular discrepancies (°) between target and replicated positions serving as the joint repositioning error [28].
Procedure
The DKV was initially assessed using the single-leg squat test [29]. To assess DKV, anatomical landmarks including the anterior superior iliac spine (ASIS), midpoint of the patella, and midpoint between the medial and lateral malleoli were marked on the frontal plane. The DKV angle was measured by drawing two lines: one from the ASIS to the patella center and another from the patella center to the intermalleolar midpoint. Participants were positioned with arms crossed and trunk upright, then asked to flex their knees to 60°, guided by a goniometer (Model 12–1027, USA) placed laterally along the femoral-tibial axis. This procedure was repeated for the surgically treated limb, with the contralateral limb flexed to approximately 60° without contact or rotation. Frontal plane photographs (Canon camera, Japan) captured knee alignment during flexion. Each trial was performed three times, with the mean angle recorded as the final DKV angle. Participants with mean DKV angle values between 16.3° and 32.4° were included in the study [30].
Participants were then assessed for baseline lower-limb kinematics by LESS [26]. Moreover, dynamic balance and knee proprioception were assessed by the Y-balance test and knee repositioning error. Following group allocation, a pre-test assessment of the LESS was conducted for both groups. The LESS was administered and scored according to the standardized criteria proposed by Padua et al. [31], with higher scores reflecting poorer landing technique. The mean score of three jumps was recorded as the final score for each participant. Participants performed a jump from a 30 cm platform, landing approximately 50% of their height away from the platform, followed by an immediate vertical jump. During training, emphasis was placed on maximizing upward movement post-landing. No feedback was provided during testing unless the participant performed the jump incorrectly.
After the instruction, participants were allowed two practice jumps to familiarize themselves with the protocol, followed by three recorded jumps. Any jump not meeting the specified horizontal distance or failing to achieve maximum vertical jump post-landing was repeated. Two tripod-mounted cameras (Canon MD 255, Japan) captured frontal and sagittal views from distances of 4.8 and 4 m, respectively. After completing the baseline assessments, the functional fatigue protocol was applied, involving the jumping exercise to induce fatigue. Post-fatigue assessments were conducted immediately afterward to evaluate any changes in kinematics, dynamic balance, and proprioception. The order of the post-fatigue assessments was consistent for all participants: kinematics were assessed first, followed by dynamic balance and then proprioception tasks. This order was chosen to standardize testing, and assessments were performed immediately after the fatigue protocol to minimize the potential effects of recovery.
Data analysis
In the statistical analysis, the normality of the data (mean and standard deviation) was initially assessed using skewness and kurtosis tests. Subsequently, for inferential statistics, a one-way analysis of variance (repeated measure) and the Bonferroni post hoc test were employed. All analyses were conducted using SPSS statistical software version 27, with a significance level set at p ≤ 0.05.