Our systematic review and meta-analysis analyzed data from 16 observational studies, which included data from 324,331 participants, to evaluate the association between exposure to environmental toxic metals, specifically cadmium, arsenic, lead, and mercury, and the risk of cardiovascular events, including stroke, cardiovascular disease (CVD), and coronary heart disease (CHD). Overall, our results revealed that individuals exposed to these toxicants exhibited greater chances of cardiovascular events. Notably, cadmium exposure was consistently associated with higher cardiovascular risk across all three outcomes: stroke, CVD, and CHD. Arsenic exposure was also significantly associated with CVD, though based on fewer studies. Lead and mercury exposure show a statistically significant association with CVD; however, neither of them has sufficient evidence to determine any association between ff and CHD individually.
Toxic metals such as cadmium and arsenic induce oxidative stress, systemic inflammation, and endothelial dysfunction, which are key processes in the pathogenesis of atherosclerosis and subsequent cardiovascular events [25, 26]. A common mechanism for metals to cause such disastrous effects involves replacing vital divalent cations [27, 28]. Cadmium especially replaces zinc in numerous enzymes and metalloproteins in the soft tissues, liver, and kidneys, leaving the proteins dysfunctional. This substitution disrupts the function of zinc-dependent enzymes and antioxidant systems, such as superoxide dismutase (SOD), which plays a crucial role in neutralizing reactive oxygen species (ROS). As a result, cadmium exposure leads to increased oxidative stress and lipid peroxidation, damaging vascular endothelial cells and accelerating the development of atherosclerosis, a central mechanism in the pathogenesis of cardiovascular diseases.
Additionally, cadmium may be taken up by several transport proteins, including calcium channels, into the cells of the immune system and infiltrate into vessel walls through cadmium-laden monocytes [29]. The increased production of monocytes and macrophages owing to cadmium may play a significant role in the development and progression of atherosclerosis due to their pivotal roles in the transdifferentiation into foam cells and subsequent necrotic foam cell death, which contributes to endothelial dysfunction. Cadmium-induced endothelial death is the fundamental mechanism by which cadmium causes atherosclerosis, which ultimately leads to CVD. Since it also raises many pro-inflammatory cytokines, including interleukin (IL)−6, IL-8, IL-1β, and tumor necrosis factor-alpha, atherosclerosis is hyperactivated by such an inflammatory response [30,31,32].
Arsenic is one of the significant clinical concerns regarding elemental toxicities [33]. The endothelium is the vasculature’s most vulnerable target for arsenic toxicity. Endothelial dysfunction initiates the development of chronic vascular abnormalities linked to atherosclerosis and cardiovascular illnesses due to an imbalance between vasoconstricting and vasodilating forces [34,35,36]. Moreover, arsenic induces ROS accumulation by binding to sulfhydryl groups of glutathione, decreasing cardiac glutathione-1 (13) [37]. The reactive oxidation species impair vasodilation by lowering NO and increasing angiotensin II (ANGII) levels. An increase in angiotensin II causes the development of metalloproteinases, such as MMP-2 and MMP-9. It throws off the equilibrium between the endothelium and the underlying vascular smooth muscle, which leads to arterial stiffness [38].
Lead and arsenic are associated with increased levels of soluble adhesion molecules in blood [39]. A 2008 systematic review on lead exposure and cardiovascular health found that population studies demonstrated a link between lead exposure and hypertension and CVD [40]. Lead promotes oxidative stress and limits nitric oxide availability. The study showed that depressed NO availability is paradoxically associated with a marked increase in endothelial NOS (eNOS) and inducible NOS abundance in the kidney and cardiovascular tissues in lead-treated animals. Similarly, because of its strong affinity for sulfhydryl groups, mercury can inactivate a variety of enzymatic processes, amino acids, and sulfur-containing antioxidants, such as N-acetyl L-cysteine, alpha-lipoic acid, and L-glutathione. This can lead to a reduction in antioxidant defense and an increase in oxidative stress [41, 42].
Metal-specific pathways beyond oxidative stress
Although oxidative stress is a common mechanism across toxic metals, each metal also targets distinct molecular pathways that intensify cellular injury. Cadmium displaces Zinc in superoxide dismutase (SOD), impairing this key antioxidant enzyme and weakening ROS senses [43]. Arsenic promotes aberrant DNA hypermethylation via DNA methyltransferases and upregulates matrix metalloproteinase-9 (MMP-9), thereby driving extracellular matrix degradation and plaque instability [44]. Lead inhibits δ-aminolevulinic acid dehydratase (ALAD), disrupting heme synthesis and increasing pro-oxidant δ-ALA levels [45]. Mercury binds sulfahydral (-SH) groups, depletes glutathione and disrupts thiol-dependant enzymes essential for detoxification. By depleting glutathione (GSH) and impairing GSH-dependent antioxidant enzymes, mercury diminishes cellular detoxification capacity. Moreover, Hg interferes with mitochondrial respiration and calcium signaling, processes essential for vascular and neuronal integrity [46]. A comparative summary of these mechanisms is provided in (Table 3), emphasising that metal- specific molecular interaction complements oxidative stress in promoting vascular and systematic toxicity.
Table 3 Metal-specific molecular pathways contributing to toxicity
The findings of our meta-analysis are primarily consistent with previous literature examining the cardiovascular risks associated with environmental exposure to toxic metals. Prior observational studies and narrative reviews have suggested that chronic exposure to metals like cadmium, arsenic, lead, and mercury contributes to cardiovascular disease development through various mechanisms, including oxidative stress, endothelial dysfunction, and chronic inflammation, as discussed above. For instance, a meta-analysis by Chowdhury et al. [47] reported a significant positive association between toxic metal exposure and cardiovascular mortality, supporting the elevated pooled proportions observed in our analysis. Similarly, studies have linked arsenic exposure, mainly through contaminated drinking water, with an increased incidence of both stroke and coronary heart disease, findings that align with our pooled estimates despite being derived from fewer included studies [48,49,50].
Lead has also been extensively studied regarding hypertension and CVD. Several large-scale studies and reviews have found that lead exposure is associated with increased all-cause and cardiovascular mortality [51,52,53]. Our findings provide a more precise assessment of the burden of cardiovascular events among exposed groups by validating and quantifying these correlations using pooled proportions.
In contrast, while mercury exposure has been historically linked to cardiovascular toxicity in animal and experimental models, epidemiological evidence in humans remains limited and inconsistent [54, 55]. Our analysis includes only one mercury-related study, which shows a significant association with CVD [ref of this study]. This suggests that this area remains under-investigated in the human population and requires further exploration.
Significantly, our meta-analysis concentrated on pooled proportions, which give an absolute measure of event occurrence. At the same time, numerous previous studies reported effect estimates such as hazard ratios (HRs), odds ratios (ORs), or relative risks (RRs). Calculating the actual burden of CVD outcomes owing to toxic metal exposure offers a valuable perspective that would be easier to include in public health planning.
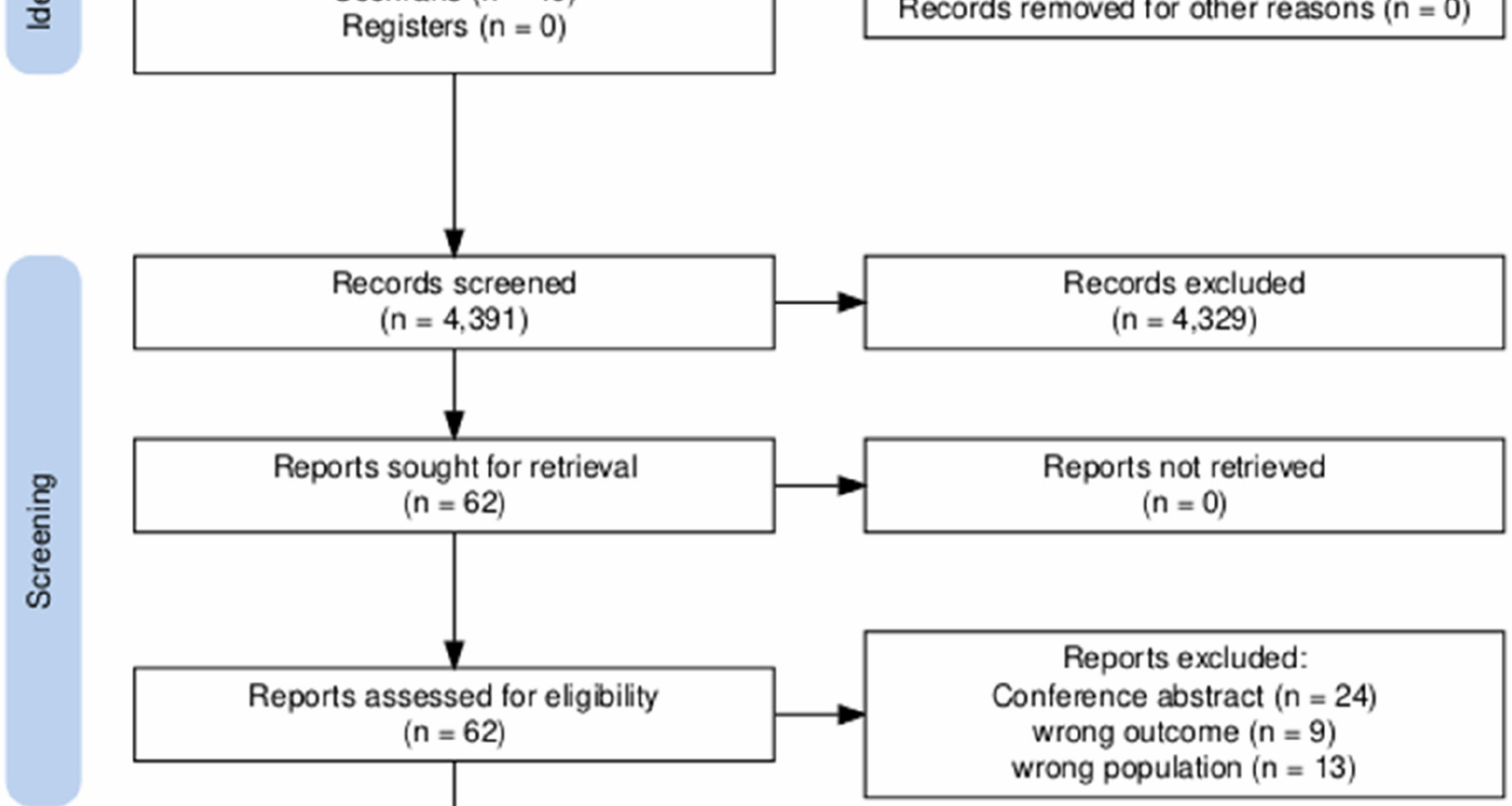
This study has several notable strengths. As an updated systematic review and meta-analysis, it provides a comprehensive and current synthesis of the available evidence, enhancing the reliability of its conclusions. All the current evidence has been pooled together, which creates this paper to be the ultimate evidence for our topic. The inclusion of a large, diverse population of over 325,000 individuals from multiple countries and several different states increases the generalizability of the findings across different healthcare settings and populations. Furthermore, the data were derived from original observational studies, including both cohort and cross-sectional designs, which reflect real-world scenarios and strengthen the external validity of the results. By integrating recent studies and applying rigorous inclusion criteria and meta-analytic methods, this review offers an updated and globally relevant perspective on our topic. Researchers and reviewers are provided with up-to-date information and insights from around the literature.
While strengths are there to be appreciated, this review has several limitations as well that should be considered when interpreting the findings. First, the inclusion was limited to English-language articles, which may have introduced language bias and excluded potentially relevant studies published in other languages. Second, although all included studies were assessed to have a low risk of bias, the absence of randomized controlled trials limits the ability to infer causality. The most important factor of all was. Substantial heterogeneity across all outcomes (I2 ≈ 99%), likely resulting from differences in study design, population characteristics, geographic settings, and outcome definitions. Despite a sensitivity analysis by the leave-one-out method being conducted, the value for heterogeneity remained high throughout. Additionally, most included studies were observational, comprising cohorts and cross-sectional studies, which, while informative for identifying associations, are limited in controlling for confounding factors. Lastly, although the studies were conducted in a diverse set of countries, including Bangladesh, the United States, Denmark, Sweden, Taiwan, Australia, Georgia, Korea, and Greenland, regions such as Africa and South America were underrepresented, which may limit the global applicability of the findings.
The findings of this study carry critical implications for public health at both national and global levels. The consistent association between exposure to environmental toxic metals and increased risk of cardiovascular and stroke-related outcomes underscores the importance of addressing environmental determinants of non-communicable diseases. Toxic metals such as lead, cadmium, arsenic, and mercury are often present in air, water, soil, and food, especially in industrialized and developing regions. Their widespread presence and potential for bioaccumulation mean that large segments of the population may be at risk, often unknowingly.
Given the observed health impacts, public health authorities need to implement and enforce stricter environmental regulations aimed at reducing metal contamination. Additionally, public health campaigns are needed to raise awareness about sources of exposure and ways to minimize risk, especially in vulnerable communities. These findings support a shift toward a more comprehensive model of cardiovascular disease prevention that includes environmental health as a core component.
While this review highlights a clear association between toxic metal exposure, several gaps in the literature remain that should be addressed in future research. First, most of the included studies were observational, which limits the ability to draw firm causal conclusions. Future investigations should prioritize longitudinal cohort studies and, where ethical and feasible, interventional trials to better establish causality. Second, there is a need for more geographically diverse data. Expanding research efforts into these underrepresented regions would enhance the global applicability of findings and ensure that local environmental and socioeconomic factors are adequately captured. Furthermore, future studies should aim to standardize methods of exposure assessment and outcome measurement to reduce heterogeneity and improve comparability across studies. Ultimately, advancing this area of research will require interdisciplinary collaboration across environmental science, epidemiology, toxicology, and public health policy to develop effective strategies for risk reduction and health risks.