Ramirez TA, Jourdan-Le SC, Joy A, Zhang J, Dai Q, Mifflin S, et al. Chronic and intermittent hypoxia differentially regulate left ventricular inflammatory and extracellular matrix responses. Hypertens Res. 2012;35(8):811–8.
Lee JW, Ko J, Ju C, Eltzschig HK. Hypoxia signaling in human diseases and therapeutic targets. Exp Mol Med. 2019;51(6):1–13.
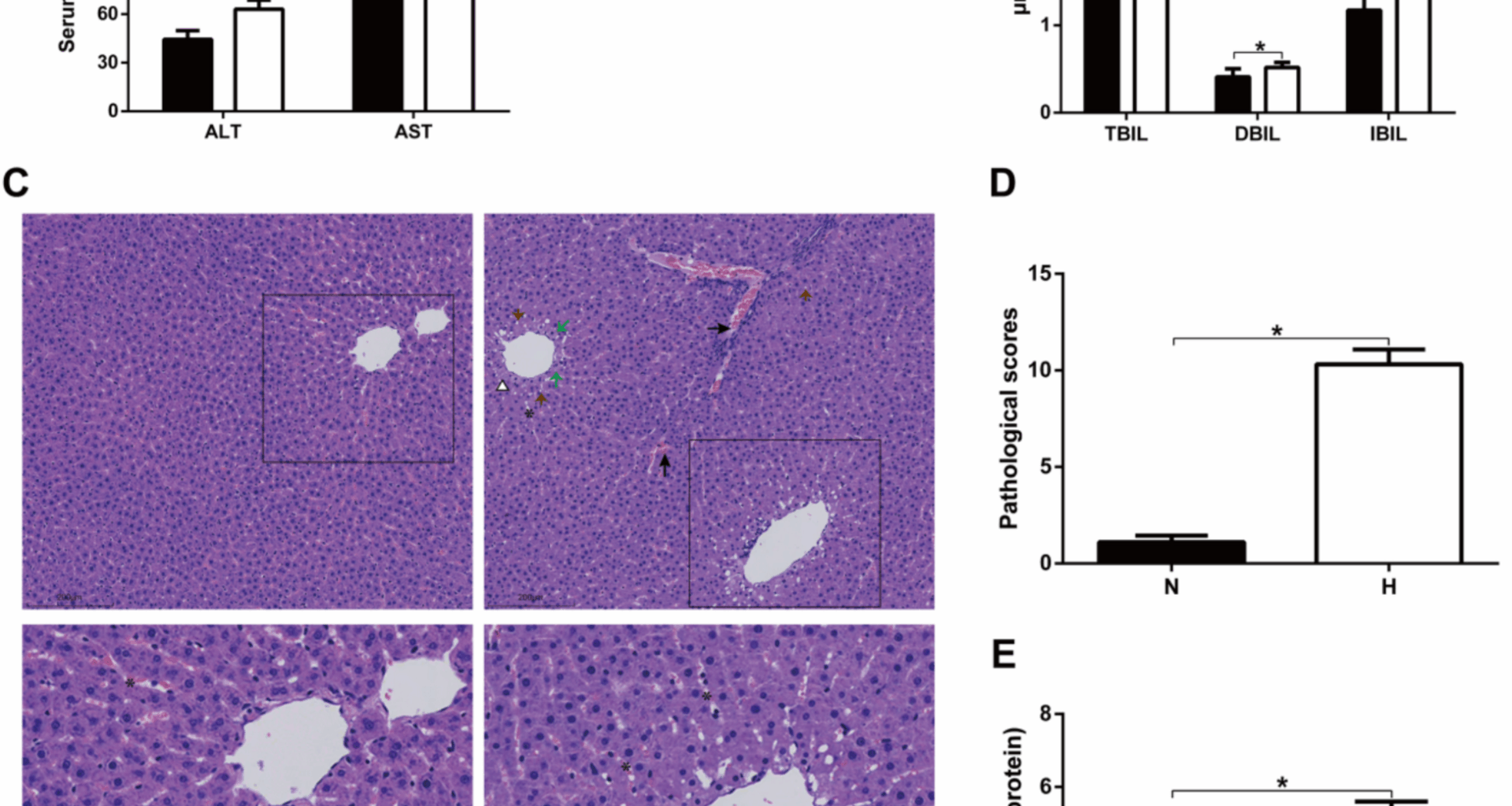
Fu Y, Zhang N, Tang W, Bi Y, Zhu D, Chu X, et al. Chronic intermittent hypoxia contributes to non-alcoholic steatohepatitis progression in patients with obesity. Hepatol Int. 2022;16(4):824–34.
Wang R, Lv Y, Ni Z, Feng W, Fan P, Wang Y, et al. Intermittent hypoxia exacerbates metabolic dysfunction-associated fatty liver disease by aggravating hepatic copper deficiency-induced ferroptosis. FASEB J. 2024;38(13):e23788.
Kudo J, Hirono H, Ohkoshi S. Low-frequency, mild-gradient chronic intermittent hypoxia still induces liver fibrogenesis in mice on a high-fat diet. Biochem Biophys Res Commun. 2025;761:151744.
Xiong Y, Wang Y, Xiong Y, Teng L. Protective effect of salidroside on hypoxia-related liver oxidative stress and inflammation via Nrf2 and JAK2/STAT3 signaling pathways. Food Sci Nutr. 2021;9(9):5060–9.
Das KK, Jargar JG, Saha S, Yendigeri SM, Singh SB. Alpha-tocopherol supplementation prevents lead acetate and hypoxia-induced hepatic dysfunction. Indian J Pharmacol. 2015;47(3):285–91.
Xiong Y, Wang Y, Xiong Y, Teng L. 4-PBA inhibits hypoxia-induced lipolysis in rat adipose tissue and lipid accumulation in the liver through regulating ER stress. Food Sci Nutr. 2023;11(3):1223–31.
O’Brien KA, McNally BD, Sowton AP, Murgia A, Armitage J, Thomas LW, et al. Enhanced hepatic respiratory capacity and altered lipid metabolism support metabolic homeostasis during short-term hypoxic stress. BMC Biol. 2021;19(1):265.
Luo M, Li T, Sang H. The role of hypoxia-inducible factor 1alpha in hepatic lipid metabolism. J MOL MED. 2023;101(5):487–500.
Gao J, Guo Z, Zhao M, Cheng X, Jiang X, Liu Y, et al. Lipidomics and mass spectrometry imaging unveil alterations in mice hippocampus lipid composition exposed to hypoxia. J Lipid Res. 2024;65(7):100575.
Hayakawa J, Wang M, Wang C, Han RH, Jiang ZY, Han X. Lipidomic analysis reveals significant lipogenesis and accumulation of lipotoxic components in ob/ob mouse organs. PROSTAG LEUKOTR ESS. 2018;136:161–9.
Chaurasia B, Tippetts TS, Mayoral MR, Liu J, Li Y, Wang L, et al. Targeting a ceramide double bond improves insulin resistance and hepatic steatosis. Science. 2019;365(6451):386–92.
Simon J, Ouro A, Ala-Ibanibo L, Presa N, Delgado TC, Martinez-Chantar ML. Sphingolipids in non-alcoholic fatty liver disease and hepatocellular carcinoma: ceramide turnover. Int J Mol Sci. 2019. https://doi.org/10.3390/ijms21010040.
Tsukamoto S, Hirotsu K, Kumazoe M, Goto Y, Sugihara K, Suda T, et al. Green tea polyphenol EGCG induces lipid-raft clustering and apoptotic cell death by activating protein kinase Cdelta and acid sphingomyelinase through a 67 kDa laminin receptor in multiple myeloma cells. Biochem J. 2012;443(2):525–34.
Zeidan YH, Hannun YA. Activation of acid sphingomyelinase by protein kinase Cdelta-mediated phosphorylation. J Biol Chem. 2007;282(15):11549–61.
Chung HY, Witt CJ, Jbeily N, Hurtado-Oliveros J, Giszas B, Lupp A, et al. Acid sphingomyelinase inhibition prevents development of sepsis sequelae in the murine liver. Sci Rep. 2017;7(1):12348.
Obuchowicz E, Prymus A, Bielecka AM, Drzyzga L, Paul-Samojedny M, Kot M, et al. Desipramine administered chronically inhibits lipopolysaccharide-stimulated production of IL-1beta in the brain and plasma of rats. Cytokine. 2016;80:26–34.
Huang M, Tang SN, Upadhyay G, Marsh JL, Jackman CP, Srivastava RK, et al. Rottlerin suppresses growth of human pancreatic tumors in nude mice, and pancreatic cancer cells isolated from Kras(G12D) mice. Cancer Lett. 2014;353(1):32–40.
Nair AB, Jacob S. A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm. 2016;7(2):27–31.
Min M, Yan BX, Wang P, Landeck L, Chen JQ, Li W, et al. Rottlerin as a therapeutic approach in psoriasis: evidence from in vitro and in vivo studies. PLoS ONE. 2017;12(12):e190051.
Sharma M, Naura AS, Singla SK. Modulatory effect of 4-phenyl butyric acid on hyperoxaluria-induced renal injury and inflammation. Mol Cell Biochem. 2019;451(1–2):185–96.
Wu Y, Adi D, Long M, Wang J, Liu F, Gai MT, et al. 4-phenylbutyric acid induces protection against pulmonary arterial hypertension in rats. PLoS ONE. 2016;11(6):e157538.
Zhang P, Qin Y, Wang H, Wang J. Vagus nerve stimulation alleviates myocardial injury following hepatic ischemia-reperfusion in rats by inhibiting ferroptosis via the activation of the SLC7A11/GPX4 axis. Eur J Med Res. 2025;30(1):162.
Ates B, Dogru MI, Gul M, Erdogan A, Dogru AK, Yilmaz I, et al. Protective role of caffeic acid phenethyl ester in the liver of rats exposed to cold stress. FUND CLIN PHARMACOL. 2006;20(3):283–9.
Shaker NS, Sahib HB. Fraxin in combination with dexamethasone attenuates LPS-induced liver and heart injury and their anticytokine activity in mice. Adv Virus Res. 2023;2023:5536933.
Zhou X, Zhao R, Lv M, Xu X, Liu W, Li X, et al. ACSL4 promotes microglia-mediated neuroinflammation by regulating lipid metabolism and VGLL4 expression. Brain Behav Immun. 2023;109:331–43.
Guo HZ, Feng RX, Zhang YJ, Yu YH, Lu W, Liu JJ, et al. A CD36-dependent non-canonical lipid metabolism program promotes immune escape and resistance to hypomethylating agent therapy in AML. Cell Rep Med. 2024;5(6):101592.
Liu Z, Xu P, Gong F, Tan Y, Han J, Tian L, et al. Altered lipidomic profiles in lung and serum of rat after sub-chronic exposure to ozone. Sci Total Environ. 2022;806(Pt 2):150630.
Chaurasia B, Summers SA. Ceramides in metabolism: key lipotoxic players. Annu Rev Physiol. 2021;83:303–30.
Pewzner-Jung Y, Park H, Laviad EL, Silva LC, Lahiri S, Stiban J, Erez-Roman R, Brugger B, Sachsenheimer T, Wieland F et al. A critical role for ceramide synthase 2 in liver homeostasis: I. alterations in lipid metabolic pathways. J Biol Chem. 2010;285(14):10902–10.
Khallaf W, Taha A, Ahmed AS, Hassan M, Abo-Youssef AM, Hemeida R. Sildenafil abrogates radiation-induced hepatotoxicity in animal model: the impact of NF-kappaB-p65, P53, Nrf2, and SIRT 1 pathway. Food Chem Toxicol. 2025;200:115373.
Shiga Y, Rangel OA, El HS, Belforte N, Quintero H, Dotigny F, et al. Endoplasmic reticulum stress-related deficits in calcium clearance promote neuronal dysfunction that is prevented by SERCA2 gene augmentation. Cell Rep Med. 2024;5(12):101839.
Bednarski TK, Rahim M, Hasenour CM, Banerjee DR, Trenary IA, Wasserman DH, et al. Pharmacological SERCA activation limits diet-induced steatohepatitis and restores liver metabolic function in mice. J Lipid Res. 2024;65(6):100558.
Ibrahim E, Sohail SK, Ihunwo A, Eid RA, Al-Shahrani Y, Rezigalla AA. Effect of high-altitude hypoxia on function and cytoarchitecture of rats’ liver. Sci Rep. 2025;15(1):12771.
Liu J, Zhao J, He J, Li Y, Xu J, Xiao C, et al. Hepcidin mediates the disorder of iron homeostasis and mitochondrial function in mice under hypobaric hypoxia exposure. Apoptosis. 2025;30(3–4):1076–91.
Zhen X, Moya EA, Gautane M, Zhao H, Lawrence ES, Gu W, et al. Combined intermittent and sustained hypoxia is a novel and deleterious cardio-metabolic phenotype. Sleep. 2022. https://doi.org/10.1093/sleep/zsab290.
Wagih SS, Abd EM, Abdel RA, Yousef AM, El SW. Clinical spectrum of nonalcoholic fatty liver disease in patients with chronic obstructive pulmonary disease. Turk Thorac J. 2022;23(6):420–5.
Suzuki K, Claggett B, Minamisawa M, Packer M, Zile MR, Rouleau J, et al. Liver function and prognosis, and influence of sacubitril/valsartan in patients with heart failure with reduced ejection fraction. Eur J Heart Fail. 2020;22(9):1662–71.
Cao Y, Wang Y, Zhou Z, Pan C, Jiang L, Zhou Z, et al. Liver-heart cross-talk mediated by coagulation factor XI protects against heart failure. Science. 2022;377(6613):1399–406.
Wang F, So KF, Xiao J, Wang H. Organ-organ communication: the liver’s perspective. Theranostics. 2021;11(7):3317–30.
Royo F, Moreno L, Mleczko J, Palomo L, Gonzalez E, Cabrera D, et al. Hepatocyte-secreted extracellular vesicles modify blood metabolome and endothelial function by an arginase-dependent mechanism. SCI REP-UK. 2017;7:42798.
Njoku DB, Schilling JD, Finck BN. Mechanisms of nonalcoholic steatohepatitis-associated cardiomyopathy: key roles for liver-heart crosstalk. CURR OPIN LIPIDOL. 2022;33(5):295–9.
Peng Z, Duggan MR, Dark HE, Daya GN, An Y, Davatzikos C, et al. Association of liver disease with brain volume loss, cognitive decline, and plasma neurodegenerative disease biomarkers. Neurobiol Aging. 2022;120:34–42.
Marra F, Svegliati-Baroni G. Lipotoxicity and the gut-liver axis in NASH pathogenesis. J Hepatol. 2018;68(2):280–95.
Sherpa LY. Deji, Stigum H, Chongsuvivatwong V, Luobu O, Thelle DS, Nafstad P, Bjertness E: Lipid profile and its association with risk factors for coronary heart disease in the highlanders of Lhasa. Tibet HIGH ALT MED BIOL. 2011;12(1):57–63.
Baracco R, Mohanna S, Seclen S. A comparison of the prevalence of metabolic syndrome and its components in high and low altitude populations in Peru. Metab Syndr Relat Disord. 2007;5(1):55–62.
Choi RH, Tatum SM, Symons JD, Summers SA, Holland WL. Ceramides and other sphingolipids as drivers of cardiovascular disease. Nat Rev Cardiol. 2021;18(10):701–11.
Katz MG, Hadas Y, Vincek A, Freage-Kahn L, Shtraizent N, Madjarov JM, et al. Acid ceramidase gene therapy ameliorates pulmonary arterial hypertension with right heart dysfunction. Respir Res. 2023;24(1):197.
Schmidt S, Gallego SF, Zelnik ID, Kovalchuk S, Albaek N, Sprenger RR, et al. Silencing of ceramide synthase 2 in hepatocytes modulates plasma ceramide biomarkers predictive of cardiovascular death. MOL THER. 2022;30(4):1661–74.
Guo L, Tan G, Liu P, Li H, Tang L, Huang L, et al. Three plasma metabolite signatures for diagnosing high altitude pulmonary edema. Sci Rep. 2015;5:15126.
Vrentzos E, Ikonomidis I, Pavlidis G, Katogiannis K, Korakas E, Kountouri A, et al. Six-month supplementation with high dose coenzyme Q10 improves liver steatosis, endothelial, vascular and myocardial function in patients with metabolic-dysfunction associated steatotic liver disease: a randomized double-blind, placebo-controlled trial. Cardiovasc Diabetol. 2024;23(1):245.
Shou JW, Ma J, Wang X, Li XX, Chen SC, Kang BH, et al. Free cholesterol-induced liver injury in non-alcoholic fatty liver disease: mechanisms and a therapeutic intervention using dihydrotanshinone I. Adv Sci. 2025;12(2):e2406191.
Wang Z, Wang Z, Lin M, Zheng B, Zhang J. A study on cholesterol-cholesteryl ester metabolic homeostasis and drug intervention in hyperlipidemic hamsters using UHPLC-MS/MS. J PHARMACEUT BIOMED. 2024;240:115933.
Sazaki I, Sakurai T, Yamahata A, Mogi S, Inoue N, Ishida K, et al. Oxidized low-density lipoproteins trigger hepatocellular oxidative stress with the formation of cholesteryl ester hydroperoxide-enriched lipid droplets. Int J Mol Sci. 2023. https://doi.org/10.3390/ijms24054281.
Fox TE, Houck KL, O’Neill SM, Nagarajan M, Stover TC, Pomianowski PT, et al. Ceramide recruits and activates protein kinase C zeta (PKC zeta) within structured membrane microdomains. J Biol Chem. 2007;282(17):12450–7.
Chen TC, Lee RA, Tsai SL, Kanamaluru D, Gray NE, Yiv N, et al. An ANGPTL4-ceramide-protein kinase Czeta axis mediates chronic glucocorticoid exposure-induced hepatic steatosis and hypertriglyceridemia in mice. J Biol Chem. 2019;294(23):9213–24.
Takahashi H, Ashikawa H, Nakamura H, Murayama T. Phosphorylation and inhibition of ceramide kinase by protein kinase C-beta: their changes by serine residue mutations. Cell Signal. 2019;54:59–68.
Zeng C, Liang B, Jiang R, Shi Y, Du Y. Protein kinase C isozyme expression in right ventricular hypertrophy induced by pulmonary hypertension in chronically hypoxic rats. Mol Med Rep. 2017;16(4):3833–40.
Ajoolabady A, Kaplowitz N, Lebeaupin C, Kroemer G, Kaufman RJ, Malhi H, et al. Endoplasmic reticulum stress in liver diseases. Hepatology. 2023;77(2):619–39.
Lebeaupin C, Vallee D, Hazari Y, Hetz C, Chevet E, Bailly-Maitre B. Endoplasmic reticulum stress signalling and the pathogenesis of non-alcoholic fatty liver disease. J Hepatol. 2018;69(4):927–47.
Meares GP, Liu Y, Rajbhandari R, Qin H, Nozell SE, Mobley JA, et al. PERK-dependent activation of JAK1 and STAT3 contributes to endoplasmic reticulum stress-induced inflammation. Mol Cell Biol. 2014;34(20):3911–25.
Chen X, Zhong J, Dong D, Liu G, Yang P. Endoplasmic reticulum stress-induced CHOP inhibits PGC-1alpha and causes mitochondrial dysfunction in diabetic embryopathy. Toxicol Sci. 2017;158(2):275–85.
Kim JY, Garcia-Carbonell R, Yamachika S, Zhao P, Dhar D, Loomba R, et al. ER stress drives lipogenesis and steatohepatitis via caspase-2 activation of S1P. Cell. 2018;175(1):133–45.
Huang M, Wang Y, Wu X, Li W. Crosstalk between endoplasmic reticulum stress and ferroptosis in liver diseases. Frontiers in Bioscience-Landmark. 2024;29(6):221.
Bhattarai KR, Riaz TA, Kim HR, Chae HJ. The aftermath of the interplay between the endoplasmic reticulum stress response and redox signaling. Exp Mol Med. 2021;53(2):151–67.
Zelnik ID, Ventura AE, Kim JL, Silva LC, Futerman AH. The role of ceramide in regulating endoplasmic reticulum function. Biochimica et Biophysica Acta (BBA). 2020;1865(1):158489.
Vangheluwe P, Raeymaekers L, Dode L, Wuytack F. Modulating sarco(endo)plasmic reticulum Ca2+ ATPase 2 (SERCA2) activity: cell biological implications. Cell Calcium. 2005;38(3–4):291–302.
Solana-Manrique C, Munoz-Soriano V, Sanz FJ, Paricio N. Oxidative modification impairs SERCA activity in Drosophila and human cell models of Parkinson’s disease. Biochimica et Biophysica Acta (BBA). 2021;1867(7):166152.
Song Q, Liu H, Zhang Y, Qiao C, Ge S. Lipidomics revealed alteration of the sphingolipid metabolism in the liver of nonalcoholic steatohepatitis mice treated with Scoparone. ACS Omega. 2022;7(16):14121–7.
Mah M, Febbraio M, Turpin-Nolan S. Circulating ceramides- are origins important for sphingolipid biomarkers and treatments? FRONT ENDOCRINOL. 2021;12:684448.
Meeusen JW, Donato LJ, Bryant SC, Baudhuin LM, Berger PB, Jaffe AS. Plasma ceramides. Arterioscler Thromb Vasc Biol. 2018;38(8):1933–9.
Pan W, Dong H, Sun R, Zhao L, Sun M, Li L, et al. Plasma ceramides in relation to coronary plaque characterization determined by optical coherence tomography. J CARDIOVASC TRANSL. 2021;14(1):140–9.
Kim J, Suresh B, Lim MN, Hong SH, Kim KS, Song HE, et al. Metabolomics reveals dysregulated sphingolipid and amino acid metabolism associated with chronic obstructive pulmonary disease. INT J CHRONIC OBSTR. 2022;17:2343–53.
Wang HN, Wang Y, Zhang SY, Bai L. Emerging roles of the acid sphingomyelinase/ceramide pathway in metabolic and cardiovascular diseases: mechanistic insights and therapeutic implications. World J Cardiol. 2025;17(2):102308.
Choi BJ, Park MH, Jin HK, Bae JS. Acid sphingomyelinase as a pathological and therapeutic target in neurological disorders: focus on Alzheimer’s disease. Exp Mol Med. 2024;56(2):301–10.
Huang FC, Du Y, Zhang XF, Guan L, Liu XM, Zeng M. SiO(2) dust induces inflammation and pulmonary fibrosis in rat lungs through activation of ASMase/ceramide pathway. J APPL TOXICOL. 2023;43(9):1319–31.
Chen C, Ji Y, Liu H, Pang L, Chen J, Chen H, et al. Acid sphingomyelinase downregulation alleviates diabetic myocardial fibrosis in mice. Mol Cell Biochem. 2025. https://doi.org/10.1007/s11010-025-05206-1.
Juneja M, Kobelt D, Walther W, Voss C, Smith J, Specker E, et al. Statin and rottlerin small-molecule inhibitors restrict colon cancer progression and metastasis via MACC1. PLoS Biol. 2017;15(6):e2000784.
Du Y, Zhao Y, Li C, Zheng Q, Tian J, Li Z, et al. Inhibition of PKCdelta reduces amyloid-beta levels and reverses Alzheimer disease phenotypes. J Exp Med. 2018;215(6):1665–77.
Zhou S, Lin Q, Huang C, Luo X, Tian X, Liu C, et al. Rottlerin plays an antiviral role at early and late steps of Zika virus infection. Virol Sin. 2022;37(5):685–94.