A recent study reveals that integrating Artificial Intelligence (AI) into colon cancer diagnosis over the past five years has significantly improved the speed and accuracy of the detection of the deadly disease.
Published in the International Journal of Medical Informatics, the study highlights how AI-driven tools provide faster, more reliable, and less invasive approaches to diagnosis and treatment planning.
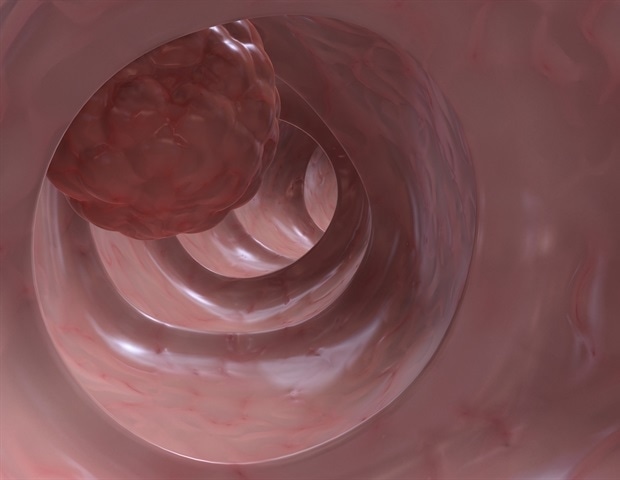
We found that AI is already making colon cancer diagnosis and prognosis more accurate, especially in identifying polyps during colonoscopy or differentiating benign from malignant tissue on pathology slides.
Our research delivers a broad and timely review of how artificial intelligence (AI), including deep learning and machine learning, has been applied to colon cancer over the past five years.”
Saad Harous, University of Sharjah’s Professor of Computing and Informatics
The findings demonstrate how AI has been applied to colon cancer via a meta-analysis of relevant studies published between 2020 and 2024. The results indicate significant improvements in diagnostic accuracy, particularly in polyp detection during colonoscopies and histopathological analysis, where deep learning approaches often outperformed traditional methods.
“Explainable AI is not just a feature. It is essential for building clinician confidence and closing the gap between technology and medical practice,” notes Prof. Harous, a co-author. “The promise of AI in medicine lies not just in speed or accuracy, but in creating transparent systems that doctors can rely on.”
The authors, affiliated with universities in Sweden, Algeria, Egypt, Saudi Arabia, and the United Arab Emirates, analyzed 80 studies, focusing on four key tasks: classification, detection, segmentation, and prediction. They examined the integration of artificial intelligence in identifying and diagnosing colon cancer, emphasizing its ability to enhance diagnostic precision, improve patient outcomes, and streamline clinical workflows. The study underscores AI’s pivotal role in transforming colon cancer care through the application of advanced diagnostic, prognostic, and segmentation models.
“The results from multiple studies demonstrate that AI enhances both diagnostic accuracy and the optimization of gland segmentation and cancer grading,” the authors write. “This has a substantial impact on precision staging and medical planning. Despite artificial intelligence (AI) systems demonstrating high accuracy and improved diagnostic capabilities, there are still persistent obstacles in terms of data diversity, model generalizability, processing demands, and the integration of segmentation models into clinical practice.”
Colorectal cancer, a common and deadly disease, is the type of cancer that affects the colon (large intestine) or rectum. It is the third most common cancer worldwide and remains a global health burden.
According to the World Health Organization (WHO), colon cancer is the second leading cause of cancer-related deaths globally, accounting for more than 930,000 deaths in 2020, a year that saw more than 1.9 million new colon cancer cases.
The study shows how AI tools are improving colon cancer care, with algorithms helping doctors find tumors and polyps earlier and with greater accuracy, offering transparency, trust, and better patient outcomes.
Prof. Harous continues, “With the promise of precision medicine, AI offers faster, more reliable, and less invasive approaches to diagnosis and treatment planning. Notably, recent work on explainable AI helps clinicians understand how these algorithms work, increasing trust and fostering adoption in real-world settings.”
The findings also highlight the remarkable progress of AI technologies for classification, prediction, segmentation, and detection of colon cancer. However, the authors point out that several challenges must be addressed, particularly in data quality, algorithm optimization, and clinical integration, before doctors reap the full benefits of AI applications in detection and diagnosis.
“Addressing these challenges is essential for AI-driven models to achieve their full potential in improving diagnostic accuracy and treatment outcomes. The need for substantial, high-quality labeled datasets to train AI models, along with the necessity for robust, scalable solutions adaptable to various clinical contexts, underscores the need for further research,” the authors note.
Meanwhile, the study identifies what Prof. Harous describes as “critical gaps,” as current research often relies on limited or homogeneous datasets, lacks external validation, and is not yet fully integrated into hospital information systems.
“AI must be tested across many hospitals and patient types; current research often uses similar, small datasets,” emphasizes Prof. Harous. “While real-world impact is close, more work is needed since most AI systems are currently being used in labs and are not yet widely adopted in clinics due to missing integration and rigorous validation.”
Source:
Journal reference:
Merabet, A., et al. (2025). AI for colon cancer: A focus on classification, detection, and predictive modeling. International Journal of Medical Informatics. doi: 10.1016/j.ijmedinf.2025.106115. https://www.sciencedirect.com/science/article/pii/S1386505625003326?via%3Dihub