Dendrou CA, Fugger L, Friese MA. Immunopathology of multiple sclerosis. Nat Rev Immunol. 2015;15(9):545–58.
Dobson R, Giovannoni G. Multiple sclerosis – a review. Eur J Neurol. 2019;26(1):27–40.
Lassmann H. Multiple sclerosis pathology. Cold Spring Harb Perspect Med. 2018. https://doi.org/10.1101/cshperspect.a028936.
Kutzelnigg A, Lucchinetti CF, Stadelmann C, Brück W, Rauschka H, Bergmann M, et al. Cortical demyelination and diffuse white matter injury in multiple sclerosis. Brain. 2005;128(Pt 11):2705–12.
Soldan SS, Lieberman PM. Epstein-Barr virus and multiple sclerosis. Nat Rev Microbiol. 2023;21(1):51–64.
Bjornevik K, Cortese M, Healy BC, Kuhle J, Mina MJ, Leng Y, et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375(6578):296–301.
Tyler KL. The enigmatic links between Epstein-Barr virus infection and multiple sclerosis. J Clin Invest. 2022. https://doi.org/10.1172/JCI160468.
Vietzen H, Berger SM, Kühner LM, Furlano PL, Bsteh G, Berger T, et al. Ineffective control of Epstein-Barr-virus-induced autoimmunity increases the risk for multiple sclerosis. Cell. 2023;186(26):5705–5718.e13.
Lanz TV, Brewer RC, Ho PP, Moon JS, Jude KM, Fernandez D, et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and glialcam. Nature. 2022;603(7900):321–7.
Thomas OG, Bronge M, Tengvall K, Akpinar B, Nilsson OB, Holmgren E, et al. Cross-reactive EBNA1 immunity targets alpha-crystallin B and is associated with multiple sclerosis. Sci Adv. 2023;9(20):eadg3032.
Tengvall K, Huang J, Hellström C, Kammer P, Biström M, Ayoglu B, et al. Molecular mimicry between Anoctamin 2 and Epstein-Barr virus nuclear antigen 1 associates with multiple sclerosis risk. Proc Natl Acad Sci U S A. 2019;116(34):16955–60.
Sundström P, Nyström M, Ruuth K, Lundgren E. Antibodies to specific EBNA-1 domains and HLA DRB1*1501 interact as risk factors for multiple sclerosis. J Neuroimmunol. 2009;215(1–2):102–7.
Lindsey JW. Antibodies to the Epstein-Barr virus proteins BFRF3 and BRRF2 cross-react with human proteins. J Neuroimmunol. 2017;310:131–4.
Vietzen H, Kühner LM, Berger SM, Furlano PL, Bsteh G, Berger T, et al. Accumulation of Epstein-Barr virus-induced cross-reactive immune responses is associated with multiple sclerosis. J Clin Invest. 2024. https://doi.org/10.1172/JCI184481.
Leung CS, Maurer MA, Meixlsperger S, Lippmann A, Cheong C, Zuo J, et al. Robust t-cell stimulation by Epstein-Barr virus-transformed B cells after antigen targeting to DEC-205. Blood. 2013;121(9):1584–94.
Hong S, Zhang Z, Liu H, Tian M, Zhu X, Wang W, et al. B cells are the dominant Antigen-Presenting cells that activate Naive CD4. Immunity. 2018;49(4):695–e7084.
Choi IK, Wang Z, Ke Q, Hong M, Qian Y, Zhao X, et al. Signaling by the Epstein-Barr virus LMP1 protein induces potent cytotoxic CD4. Proc Natl Acad Sci U S A. 2018;115(4):E686–95.
Torkildsen Ø, Nyland H, Myrmel H, Myhr KM. Epstein–Barr virus reactivation and multiple sclerosis. Eur J Neurol. 2008;15(1):106–8.
Serafini B, Scorsi E, Rosicarelli B, Rigau V, Thouvenot E, Aloisi F. Massive intracerebral Epstein-Barr virus reactivation in lethal multiple sclerosis relapse after natalizumab withdrawal. J Neuroimmunol. 2017;307:14–7.
Shimakage M, Sakamoto H. Macrophage involvement in Epstein-Barr virus-related tumors. Exp Ther Med. 2010;1(2):285–91.
Wang J, Su M, Wei N, Yan H, Zhang J, Gong Y, et al. Chronic active Epstein-Barr virus disease originates from infected hematopoietic stem cells. Blood. 2024;143(1):32–41.
Yu H, Robertson ES. Epstein-Barr virus history and pathogenesis. Viruses. 2023. https://doi.org/10.3390/v15030714.
Kempkes B, Robertson ES. Epstein-barr virus latency: current and future perspectives. Curr Opin Virol. 2015;14:138–44.
Mrozek-Gorska P, Buschle A, Pich D, Schwarzmayr T, Fechtner R, Scialdone A, et al. Epstein-Barr virus reprograms human B lymphocytes immediately in the prelatent phase of infection. Proc Natl Acad Sci U S A. 2019;116(32):16046–55.
Münz C. Latency and lytic replication in Epstein-barr virus-associated oncogenesis. Nat Rev Microbiol. 2019;17(11):691–700.
Kenney SC, Mertz JE. Regulation of the latent-lytic switch in Epstein-Barr virus. Semin Cancer Biol. 2014;26:60–8.
Moreno MA, Or-Geva N, Aftab BT, Khanna R, Croze E, Steinman L, et al. Molecular signature of Epstein-Barr virus infection in MS brain lesions. Neurol Neuroimmunol Neuroinflamm. 2018;5(4):e466.
Serafini B, Rosicarelli B, Franciotta D, Magliozzi R, Reynolds R, Cinque P, et al. Dysregulated Epstein-Barr virus infection in the multiple sclerosis brain. J Exp Med. 2007;204(12):2899–912.
Hassani A, Corboy JR, Al-Salam S, Khan G. Epstein-Barr virus is present in the brain of most cases of multiple sclerosis and may engage more than just B cells. PLoS One. 2018;13(2):e0192109.
Orr N, Steinman L. Epstein-Barr virus and the immune microenvironment in multiple sclerosis: insights from high-dimensional brain tissue imaging. Proc Natl Acad Sci U S A. 2025;122(11):e2425670122.
Pike SC, Welsh N, Linzey M, Gilli F. Theiler’s virus-induced demyelinating disease as an infectious model of progressive multiple sclerosis. Front Mol Neurosci. 2022;15:1019799.
Matthews AE, Weiss SR, Paterson Y. Murine hepatitis virus–a model for virus-induced CNS demyelination. J Neurovirol. 2002;8(2):76–85.
Mokhtarian F, Huan CM, Roman C, Raine CS. Semliki forest virus-induced demyelination and remyelination–involvement of B cells and anti-myelin antibodies. J Neuroimmunol. 2003;137(1–2):19–31.
Olson JK, Croxford JL, Calenoff MA, Dal Canto MC, Miller SD. A virus-induced molecular mimicry model of multiple sclerosis. J Clin Invest. 2001;108(2):311–8.
Axthelm MK, Bourdette DN, Marracci GH, Su W, Mullaney ET, Manoharan M, et al. Japanese macaque encephalomyelitis: a spontaneous multiple sclerosis-like disease in a nonhuman primate. Ann Neurol. 2011;70(3):362–73.
Yong VW. Microglia in multiple sclerosis: protectors turn destroyers. Neuron. 2022;110(21):3534–48.
Distéfano-Gagné F, Bitarafan S, Lacroix S, Gosselin D. Roles and regulation of microglia activity in multiple sclerosis: insights from animal models. Nat Rev Neurosci. 2023;24(7):397–415.
Montilla A, Zabala A, Er-Lukowiak M, Rissiek B, Magnus T, Rodriguez-Iglesias N, et al. Microglia and meningeal macrophages depletion delays the onset of experimental autoimmune encephalomyelitis. Cell Death Dis. 2023;14(1):16.
van den Bosch AMR, van der Poel M, Fransen NL, Vincenten MCJ, Bobeldijk AM, Jongejan A, et al. Profiling of microglia nodules in multiple sclerosis reveals propensity for lesion formation. Nat Commun. 2024;15(1):1667.
van der Valk P, Amor S. Preactive lesions in multiple sclerosis. Curr Opin Neurol. 2009;22(3):207–13.
Gay FW, Drye TJ, Dick GW, Esiri MM. The application of multifactorial cluster analysis in the staging of plaques in early multiple sclerosis. Identification and characterization of the primary demyelinating lesion. Brain. 1997;120(Pt 8):1461–83.
Dong S, Forrest JC, Liang X. Murine gammaherpesvirus 68: a small animal model for gammaherpesvirus-associated diseases. Adv Exp Med Biol. 2017;1018:225–36.
Caminero F, Cascella M. Neuroanatomy, mesencephalon midbrain. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
Wilkins A. Cerebellar dysfunction in multiple sclerosis. Front Neurol. 2017;8:312.
Ashizawa T, Xia G. Ataxia. Continuum. 2016;22(4 Movement Disorders):1208–26.
Terry LA, Stewart JP, Nash AA, Fazakerley JK. Murine gammaherpesvirus-68 infection of and persistence in the central nervous system. J Gen Virol. 2000;81(Pt 11):2635–43.
Kang HR, Cho HJ, Kim S, Song IH, Lee TS, Hwang S, et al. Persistent infection of a gammaherpesvirus in the central nervous system. Virology. 2012;423(1):23–9.
Collins CM, Speck SH. Tracking murine gammaherpesvirus 68 infection of germinal center B cells in vivo. PLoS One. 2012;7(3):e33230.
Casiraghi C, Shanina I, Cho S, Freeman ML, Blackman MA, Horwitz MS. Gammaherpesvirus latency accentuates EAE pathogenesis: relevance to Epstein-Barr virus and multiple sclerosis. PLoS Pathog. 2012;8(5):e1002715.
Casiraghi C, Márquez AC, Shanina I, Horwitz MS. Latent virus infection upregulates CD40 expression facilitating enhanced autoimmunity in a model of multiple sclerosis. Sci Rep. 2015;5:13995.
Perry VH, Holmes C. Microglial priming in neurodegenerative disease. Nat Rev Neurol. 2014;10(4):217–24.
Neher JJ, Cunningham C. Priming microglia for innate immune memory in the brain. Trends Immunol. 2019;40(4):358–74.
Lima MN, Barbosa-Silva MC, Maron-Gutierrez T. Microglial priming in infections and its risk to neurodegenerative diseases. Front Cell Neurosci. 2022;16:878987.
Hoeijmakers L, Heinen Y, van Dam AM, Lucassen PJ, Korosi A. Microglial priming and Alzheimer’s disease: a possible role for (early) immune challenges and epigenetics?? Front Hum Neurosci. 2016;10:398.
Kitazawa M, Oddo S, Yamasaki TR, Green KN, LaFerla FM. Lipopolysaccharide-induced inflammation exacerbates Tau pathology by a cyclin-dependent kinase 5-mediated pathway in a transgenic model of alzheimer’s disease. J Neurosci. 2005;25(39):8843–53.
Sly LM, Krzesicki RF, Brashler JR, Buhl AE, McKinley DD, Carter DB, et al. Endogenous brain cytokine mRNA and inflammatory responses to lipopolysaccharide are elevated in the Tg2576 transgenic mouse model of Alzheimer’s disease. Brain Res Bull. 2001;56(6):581–8.
Ramaglia V, Hughes TR, Donev RM, Ruseva MM, Wu X, Huitinga I, et al. C3-dependent mechanism of microglial priming relevant to multiple sclerosis. Proc Natl Acad Sci U S A. 2012;109(3):965–70.
Bilbo SD, Levkoff LH, Mahoney JH, Watkins LR, Rudy JW, Maier SF. Neonatal infection induces memory impairments following an immune challenge in adulthood. Behav Neurosci. 2005;119(1):293–301.
Ratnayake U, Quinn T, Walker DW, Dickinson H. Cytokines and the neurodevelopmental basis of mental illness. Front Neurosci. 2013;7:180.
Li WY, Chang YC, Lee LJ. Prenatal infection affects the neuronal architecture and cognitive function in adult mice. Dev Neurosci. 2014;36(5):359–70.
Granja MG, Alves LP, Leardini-Tristão M, Saul ME, Bortoni LC, de Moraes FM, et al. Inflammatory, synaptic, motor, and behavioral alterations induced by gestational sepsis on the offspring at different stages of life. J Neuroinflammation. 2021;18(1):60.
Kuhlmann T, Ludwin S, Prat A, Antel J, Brück W, Lassmann H. An updated histological classification system for multiple sclerosis lesions. Acta Neuropathol. 2017;133(1):13–24.
Lucchinetti C, Brück W, Parisi J, Scheithauer B, Rodriguez M, Lassmann H. Heterogeneity of multiple sclerosis lesions: implications for the pathogenesis of demyelination. Ann Neurol. 2000;47(6):707–17.
Schetters STT, Gomez-Nicola D, Garcia-Vallejo JJ, Van Kooyk Y. Neuroinflammation: microglia and T cells get ready to Tango. Front Immunol. 2017;8:1905.
van Nierop GP, van Luijn MM, Michels SS, Melief MJ, Janssen M, Langerak AW, et al. Phenotypic and functional characterization of T cells in white matter lesions of multiple sclerosis patients. Acta Neuropathol. 2017;134(3):383–401.
Pierson E, Simmons SB, Castelli L, Goverman JM. Mechanisms regulating regional localization of inflammation during CNS autoimmunity. Immunol Rev. 2012;248(1):205–15.
Goverman J. Autoimmune T cell responses in the central nervous system. Nat Rev Immunol. 2009;9(6):393–407.
Snyder-Keller A, Bolivar VJ, Zink S, Kramer LD. Brain iron accumulation and the formation of calcifications after developmental Zika virus infection. J Neuropathol Exp Neurol. 2020;79(7):767–76.
Wang MP, Joshua B, Jin NY, Du SW, Li C. Ferroptosis in viral infection: the unexplored possibility. Acta Pharmacol Sin. 2022;43(8):1905–15.
Calvi A, Haider L, Prados F, Tur C, Chard D, Barkhof F. In vivo imaging of chronic active lesions in multiple sclerosis. Mult Scler. 2022;28(5):683–90.
Dal-Bianco A, Grabner G, Kronnerwetter C, Weber M, Höftberger R, Berger T, et al. Slow expansion of multiple sclerosis iron rim lesions: pathology and 7 T magnetic resonance imaging. Acta Neuropathol. 2017;133(1):25–42.
Gillen KM, Mubarak M, Nguyen TD, Pitt D. Significance and in vivo detection of iron-laden microglia in white matter multiple sclerosis lesions. Front Immunol. 2018;9:255.
Scarl RT, Lawrence CM, Gordon HM, Nunemaker CS. STEAP4: its emerging role in metabolism and homeostasis of cellular iron and copper. J Endocrinol. 2017;234(3):R123-34.
Miedema A, Gerrits E, Brouwer N, Jiang Q, Kracht L, Meijer M, et al. Brain macrophages acquire distinct transcriptomes in multiple sclerosis lesions and normal appearing white matter. Acta Neuropathol Commun. 2022;10(1):8.
Fillebeen C, Lam NH, Chow S, Botta A, Sweeney G, Pantopoulos K. Regulatory connections between iron and glucose metabolism. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21207773.
Bernier LP, York EM, Kamyabi A, Choi HB, Weilinger NL, MacVicar BA. Microglial metabolic flexibility supports immune surveillance of the brain parenchyma. Nat Commun. 2020;11(1):1559.
Lauro C, Limatola C. Metabolic reprograming of microglia in the regulation of the innate inflammatory response. Front Immunol. 2020;11:493.
Zhang S, Xin W, Anderson GJ, Li R, Gao L, Chen S, et al. Double-edge sword roles of iron in driving energy production versus instigating ferroptosis. Cell Death Dis. 2022;13(1):40.
Hider RC, Hoffbrand AV. The role of deferiprone in iron chelation. N Engl J Med. 2018;379(22):2140–50.
Yiu SPT, Hui KF, Choi CK, Kao RYT, Ma CW, Yang D, et al. Intracellular iron chelation by a novel compound, C7, reactivates epstein⁻barr virus (EBV) lytic cycle via the ERK-autophagy axis in EBV-positive epithelial cancers. Cancers (Basel). 2018. https://doi.org/10.3390/cancers10120505.
Saikawa H, Nagashima H, Maeda T, Maemondo M. Acute cerebellar ataxia due to Epstein-Barr virus under administration of an immune checkpoint inhibitor. BMJ Case Rep. 2019. https://doi.org/10.1136/bcr-2019-231520.
Keith KA, Hartline CB, Bowlin TL, Prichard MN. A standardized approach to the evaluation of antivirals against DNA viruses: polyomaviruses and lymphotropic herpesviruses. Antivir Res. 2018;159:122–9.
Coen N, Duraffour S, Naesens L, Krecmerová M, Van den Oord J, Snoeck R, et al. Evaluation of novel acyclic nucleoside phosphonates against human and animal gammaherpesviruses revealed an altered metabolism of Cyclic prodrugs upon Epstein-Barr virus reactivation in P3HR-1 cells. J Virol. 2013;87(22):12422–32.
Coen N, Duraffour S, Topalis D, Snoeck R, Andrei G. Spectrum of activity and mechanisms of resistance of various nucleoside derivatives against gammaherpesviruses. Antimicrob Agents Chemother. 2014;58(12):7312–23.
Neyts J, De Clercq E. In vitro and in vivo inhibition of murine gamma herpesvirus 68 replication by selected antiviral agents. Antimicrob Agents Chemother. 1998;42(1):170–2.
Rouse BT, Sehrawat S. Immunity and immunopathology to viruses: what decides the outcome? Nat Rev Immunol. 2010;10(7):514–26.
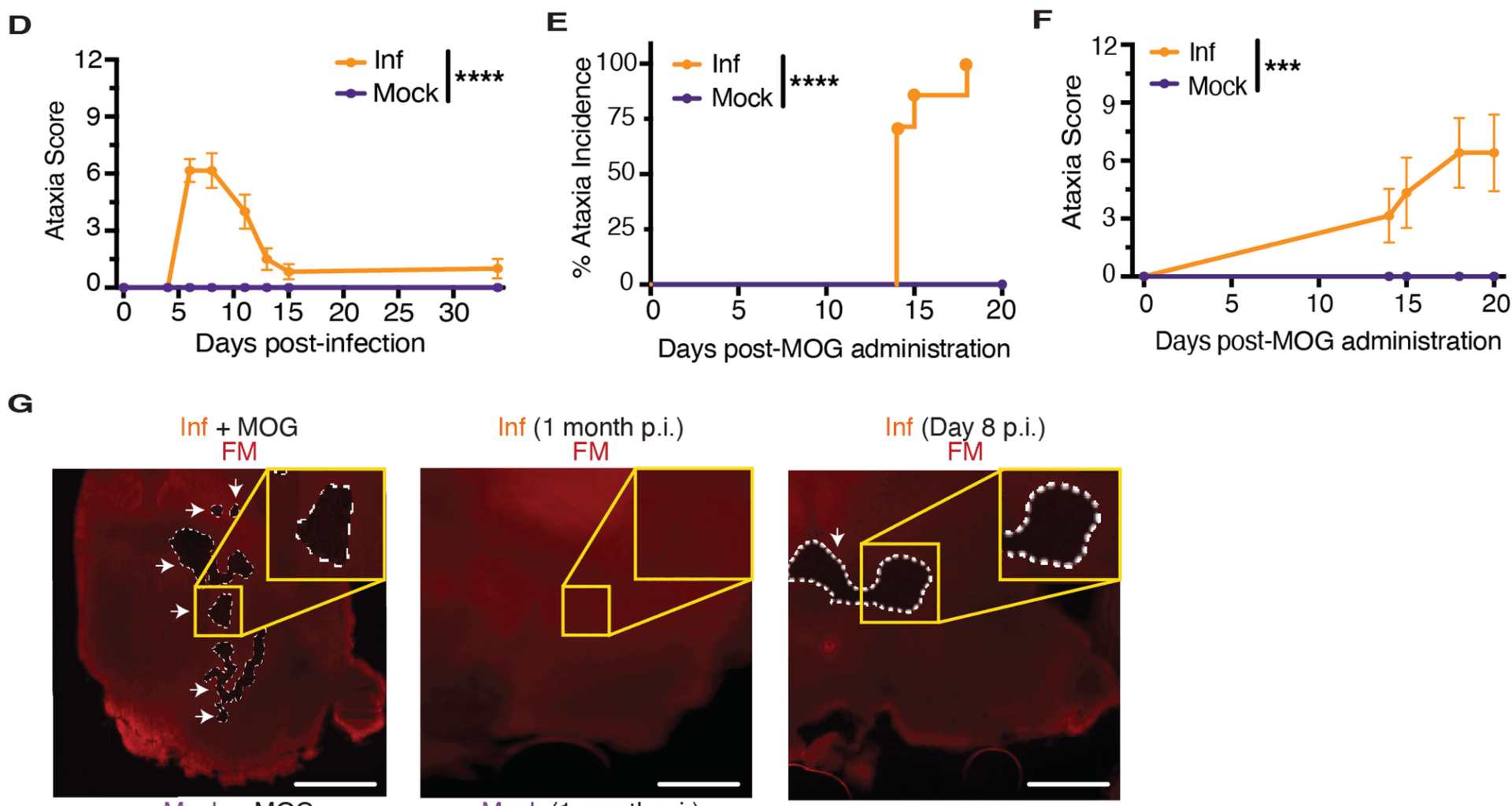
Deffenbaugh LJ, Jung K-J, Murphy PS, Liu Y, Rau NC, Petersen-Cherubini LC, et al. Novel model of multiple sclerosis induced by EBV-like virus generates a unique B cell population. J Neuroimmunol. 2024;394:578408.
Márquez AC, Horwitz MS. The role of latently infected B cells in CNS autoimmunity. Front Immunol. 2015;6:544.
Taylor WR, Rasley A, Bost KL, Marriott I. Murine gammaherpesvirus-68 infects microglia and induces high levels of pro-inflammatory cytokine production. J Neuroimmunol. 2003;136(1–2):75–83.
Cho HJ, Kim S, Kwak SE, Kang TC, Kim HS, Kwon HJ, et al. Age-dependent pathogenesis of murine gammaherpesvirus 68 infection of the central nervous system. Mol Cells. 2009;27(1):105–11.
Tang Y, Chaillon A, Gianella S, Wong LM, Li D, Simermeyer TL, et al. Brain microglia serve as a persistent HIV reservoir despite durable antiretroviral therapy. J Clin Invest. 2023. https://doi.org/10.1172/JCI167417.
Chivero ET, Guo ML, Periyasamy P, Liao K, Callen SE, Buch S. HIV-1 Tat primes and activates microglial NLRP3 inflammasome-mediated neuroinflammation. J Neurosci. 2017;37(13):3599–609.
Hamdy E, Galeel AA, Ramadan I, Gaber D, Mustafa H, Mekky J. Iron deposition in multiple sclerosis: overall load or distribution alteration? Eur Radiol Exp. 2022;6(1):49.
Ropele S, Enzinger C, Fazekas F. Iron mapping in multiple sclerosis. Neuroimaging Clin N Am. 2017;27(2):335–42.
Tang C, Yang J, Zhu C, Ding Y, Yang S, Xu B, et al. Iron metabolism disorder and multiple sclerosis: a comprehensive analysis. Front Immunol. 2024;15:1376838.
Zhao J, Liao Y, Miller-Little W, Xiao J, Liu C, Li X, et al. STEAP4 expression in CNS resident cells promotes Th17 cell-induced autoimmune encephalomyelitis. J Neuroinflammation. 2021;18(1):98.
Wang Z, Guo R, Trudeau SJ, Wolinsky E, Ast T, Liang JH, et al. CYB561A3 is the key lysosomal iron reductase required for Burkitt B-cell growth and survival. Blood. 2021;138(22):2216–30.
Absinta M, Sati P, Masuzzo F, Nair G, Sethi V, Kolb H, et al. Association of chronic active multiple sclerosis lesions with disability in vivo. JAMA Neurol. 2019;76(12):1474–83.
Absinta M, Sati P, Schindler M, Leibovitch EC, Ohayon J, Wu T, et al. Persistent 7-tesla phase rim predicts poor outcome in new multiple sclerosis patient lesions. J Clin Invest. 2016;126(7):2597–609.
Weigel KJ, Lynch SG, LeVine SM. Iron chelation and multiple sclerosis. ASN Neuro. 2014;6(1):e00136.
Vragel G, Gomez BD, Kostelecky RE, Noell KS, Tseng A, Cohen S et al. Murine Gammaherpesvirus 68 Efficiently Infects Myeloid Cells Resulting In An Atypical, Restricted Form Of Infection. bioRxiv. 2023.
Israel FB, Kenney CS. Virally targeted therapies for EBV-associated malignancies. Oncogene. 2003;22(33):5122–30.
Yiu TPS, Dorothea M, Hui FK, Chiang SKA. Lytic induction therapy against Epstein–Barr virus-associated malignancies: past, present, and future. Cancers. 2020;12(8):2142.
Hui KF, Chiang KSA. Suberoylanilide hydroxamic acid induces viral lytic cycle in Epstein-Barr virus‐positive epithelial malignancies and mediates enhanced cell death. Int J Cancer. 2010;126(10):2479–89.
Chakravorty S, Afzali B, Kazemian M. EBV-associated diseases: current therapeutics and emerging technologies. Front Immunol. 2022;13:1059133.
Rühl J, Leung SC, Münz C. Vaccination against the Epstein–Barr virus. Cell Mol Life Sci. 2020;77(21):4315–24.
Kanekiyo M, Bu W, Joyce GM, Meng G, Whittle RRJ, Baxa U, et al. Rational design of an Epstein-Barr virus vaccine targeting the receptor-binding site. Cell. 2015;162(5):1090–100.
Dasari V, Mcneil KL, Beckett K, Solomon M, Ambalathingal G, Thuy LT et al. Lymph node targeted multi-epitope subunit vaccine promotes effective immunity to EBV in HLA-expressing mice. Nat Commun. 2023;14(1):4371.
Maple AP, Ascherio A, Cohen IJ, Cutter G, Giovannoni G, Shannon-Lowe C, et al. The potential for EBV vaccines to prevent multiple sclerosis. Front Neurol. 2022;13:887794.
Lee KE, Kim YS, Noh K-W, Joo HE, Zhao B, Kieff E, et al. Small molecule Inhibition of Epstein–Barr virus nuclear antigen-1 DNA binding activity interferes with replication and persistence of the viral genome. Antiviral Res. 2014;104:73–83.
Kim YS, Song K-A, Kieff E, Kang M-S. Small molecule and peptide-mediated Inhibition of Epstein-Barr virus nuclear antigen 1 dimerization. Biochem Biophys Res Commun. 2012;424(2):251–6.
Alqarni S, Al-Sheikh Y, Campbell D, Drotar M, Hannigan A, Boyle S, et al. Lymphomas driven by Epstein–Barr virus nuclear antigen-1 (EBNA1) are dependant upon Mdm2. Oncogene. 2018;37(29):3998–4012.
Monaco GCM, Soldan SS, Su C, Clauze A, Cooper FJ, Patel JR, et al. EBNA1 inhibitors block proliferation of spontaneous lymphoblastoid cell lines from patients with multiple sclerosis and healthy controls. Neurol Neuroimmunol Neuroinflammation. 2023;10(5):e200149.
Smith C, Khanna R. Adoptive T-cell therapy targeting Epstein–Barr virus as a treatment for multiple sclerosis. Clin Transl Immunol. 2023. https://doi.org/10.1002/cti2.1444.
Pender PM, Csurhes AP, Smith C, Douglas LN, Neller AM, Matthews KK, et al. Epstein-Barr virus–specific T cell therapy for progressive multiple sclerosis. JCI Insight. 2018;3(22):e124714.
Colón Ortiz C, Eroglu C. Astrocyte signaling and interactions in multiple sclerosis. Curr Opin Cell Biol. 2024;86:102307.
Aharoni R, Eilam R, Arnon R. Astrocytes in multiple sclerosis-essential constituents with diverse multifaceted functions. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22115904.
Dulamea AO. Role of oligodendrocyte dysfunction in demyelination, remyelination and neurodegeneration in multiple sclerosis. Adv Exp Med Biol. 2017;958:91–127.
Pan R, Zhang Q, Anthony SM, Zhou Y, Zou X, Cassell M, et al. Oligodendrocytes that survive acute coronavirus infection induce prolonged inflammatory responses in the CNS. Proc Natl Acad Sci U S A. 2020;117(27):15902–10.
Blackhurst BM, Funk KE. Viral pathogens increase risk of neurodegenerative disease. Nat Rev Neurol. 2023;19(5):259–60.
Huang SY, Yang YX, Kuo K, Li HQ, Shen XN, Chen SD, et al. Herpesvirus infections and Alzheimer’s disease: a Mendelian randomization study. Alzheimers Res Ther. 2021;13(1):158.
Tiwari D, Mittal N, Jha HC. Unraveling the links between neurodegeneration and Epstein-Barr virus-mediated cell cycle dysregulation. Curr Res Neurobiol. 2022;3:100046.
Manoharan S, Ying LY. Epstein barr virus reactivation during COVID-19 hospitalization significantly increased mortality/death in SARS-CoV-2(+)/EBV(+) than SARS-CoV-2(+)/EBV(-) patients: A comparative Meta-Analysis. Int J Clin Pract. 2023;2023:1068000.
Maniscalco GT, Dinoto A, Foglia MC, Di Battista ME, Moreggia O, Di Giulio Cesare D, et al. Epstein-barr virus infection in patients with MOGAD. Mult Scler. 2025;31(1):117–20.
Fadda G, Yea C, O’Mahony J, Waters P, Yeh EA, Marrie RA, et al. Epstein-Barr virus strongly associates with pediatric multiple sclerosis, but not Myelin oligodendrocyte Glycoprotein-Antibody-Associated disease. Ann Neurol. 2024;95(4):700–5.
Sunil-Chandra NP, Efstathiou S, Arno J, Nash AA. Virological and pathological features of mice infected with murine gamma-herpesvirus 68. J Gen Virol. 1992;73(Pt 9):2347–56.
Baer A, Kehn-Hall K. Viral concentration determination through plaque assays: using traditional and novel overlay systems. J Vis Exp. 2014;93:e52065.
Inoue A, Koh C-S, Yamazaki M, Yahikozawa H, Ichikawa M, Yagita H, et al. Suppressive effect on theiler’s murine encephalomyelitis virus-induced demyelinating disease by the administration of anti-IL-12 antibody. J Immunol. 1998;161(10):5586–93.
Guyenet SJ, Furrer SA, Damian VM, Baughan TD, La Spada AR, Garden GA. A simple composite phenotype scoring system for evaluating mouse models of cerebellar ataxia. J Vis Exp. 2010;(39):1787.