The systematic review and meta-analysis including 21 studies indicated the participants in the highest TyG, TyG-BMI, TyG-WC and TyG-WHtR quartile have an increased risk of stroke compared to the patients with the lowest index category. Subgroup analysis showed that the association between TyG and its related parameters and the subsequent incidence of stroke was not significantly affected by the gender, region, sample size, or duration of follow-up.
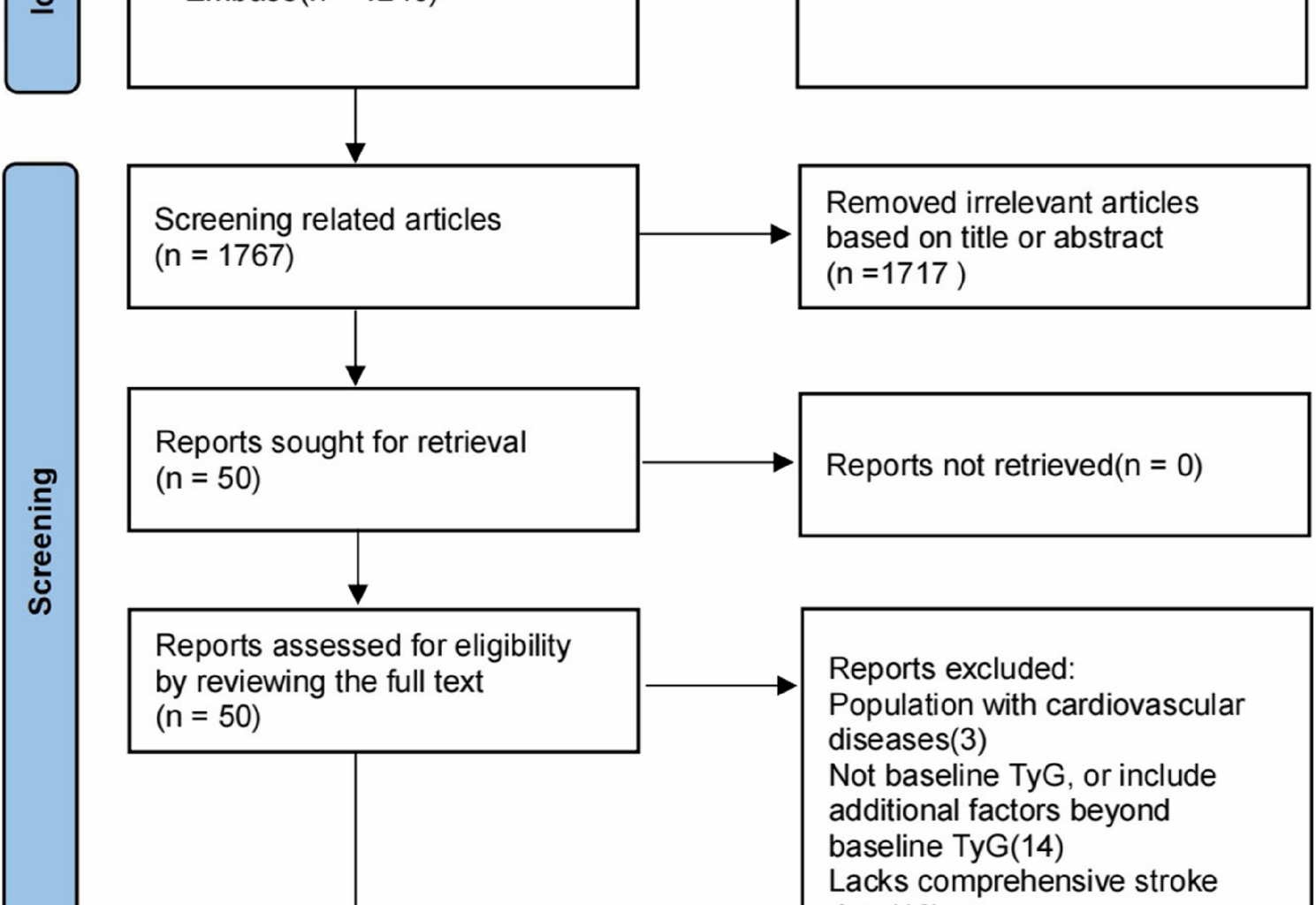
Previous studies have reported there was a positive association between the TyG index and stroke [24]. Compared to previous research, our study has several advantages. Firstly, this study is the first meta-analysis to summarize the association between the TyG-BMI, TyG-WC and TyG-WHtR index and the risk of stroke. Secondly, we included more recent studies by an updated search, which enhanced the precision of the estimated effect size. Thirdly, only cohort studies were included and HR was calculated instead of relative risk (RR), which the potential recall bias associated with cross-sectional studies was avoided and considered the time-dependent effect.
Our study found that individuals in the highest TyG quartile were at an increased risk of stroke. A previous study has suggested that the TyG index is considered as an efficient biomarker of IR [28]. IR could play a key role in stroke pathogenesis through several potential mechanisms. When insulin resistance occurs, high insulin levels can activate mitogen-activated protein kinase (MAPK), which causes vasoconstriction, proliferation of vascular smooth muscle cells, thickening of the vessel wall, and narrowing of the vessel lumen—thereby increasing blood pressure, impairing organ perfusion, and elevating CVD risk [9, 10]. IR can promote the activation of the inflammatory response with the release of inflammatory mediators and this can interfere with insulin receptor function and signaling, as well as damage vascular endothelial cells [10]. Additionally, IR can lead to an imbalance of oxidation and antioxidants in the body, resulting in excessive free radical production, which damages vascular endothelial cells and inhibits insulin signalling, thereby increasing the risk of stroke [29]. IR also leads to disturbances in glucose and lipid metabolism, and this causes lipids to deposit in the inner walls of blood vessels, leading to the formation of atherosclerotic plaques [11, 30]. Furthermore, IR increases endoplasmic reticulum stress in macrophages within plaques, leading to cell apoptosis. The uncleared apoptotic macrophages then undergo secondary necrosis, which accumulates to form a necrotic core. This process may contribute to plaque rupture and thrombosis in later stages [31]. In addition, IR is associated with hyperfibrinogenemia and enhanced platelet aggregation [13, 32]. These pathways might lead to stroke by atherosclerosis and vascular occlusion.
Our study also found that the highest TyG-BMI, TyG-WC and TyG-WHtR quartile had a higher risk of stroke. TyG combined with obesity indices including BMI, WC and WHtR, which captured multiple clinical variables, demonstrated a stronger association with IR than the individual indices [22, 33]. Dang et al. found that the TyG-WC and TyG-WHtR enhanced its ability to predict cardiovascular disease mortality [34]. The obesity indices including BMI, WC and WHtR were regarded as indicators for assessing visceral adiposity. IR and visceral adiposity dysfunction were related to chronic inflammation, vascular endothelial injury and atherosclerosis. Therefore, the potential mechanism underlying the relationship between TyG-BMI, TyG-WC and TyG-WHtR and stroke incidence may be related to the association of insulin sensitivity and excessive accumulation of visceral adiposity.
It has been suggested that sex hormones may contribute to IR by affecting fat distribution, inflammatory responses, and metabolic pathways [35]. An analysis based on the I-Lan Longitudinal Aging Study (ILAS) revealed a notable gender difference in the correlation between a high TyG index (≥ 8.55) and subclinical atherosclerosis (SA) in patients without diabetes. After adjusting for traditional risk factors, a high TyG index was found to be an independent predictor of SA in nondiabetic women (OR = 1.51, 95% CI: 1.01–2.26), whereas this association was not statistically significant in men [36]. The present meta-analysis, based on a subgroup analysis of populations in which more than half were of one sex or the other, found that high TyG and TyG-BMI parameters were more predictive of stroke risk in men than in women, whereas high TyG-WC and TyG-WHtR parameters were less predictive. The literature was searched for possible reasons for the gender differences observed, but little relevant literature was found. Further investigation of gender differences in the correlation between TyG and related parameters and stroke is needed in order to utilise them more effectively in clinical practice.
There were several limitations that should be considered in our study. First, of the 21 included studies, 18 were conducted in Asia, and only 3 studies were from Western countries. The studies exploring the association between TyG-BMI, TyG-WC, and TyG-WHtR parameters and stroke were all from Asia. However, there are differences in genetic background, dietary structure, and healthcare resource allocation among populations of different races and regions. These differences may affect the generalizability of the association between the TyG and related parameters and stroke. For instance, genetic polymorphisms may affect stroke susceptibility by regulating lipid metabolism or insulin sensitivity, leading to differences in TyG index among different races and populations. A study based on the United States National Health and Nutrition Examination Survey (NHANES) cohort showed that TyG index was more strongly associated with stroke risk among non-Hispanic whites, possibly related to the distribution of their genetic polymorphisms [37].Comparative analyses of the Western diet and the Mediterranean diet found that the “Westernized diet”, which is based on animal fats and preserved foods, was significantly positively associated with TG, fasting blood sugar(FBS), and TyG index [38], whereas the Mediterranean diet reduces the progression rate of carotid intima-media thickness and reduces the risk of cardiovascular events, and its cardiovascular protective effects may improve insulin sensitivity through high intake of monounsaturated fatty acids and dietary fiber, which in turn reduces the TyG index [39]. In addition, areas with insufficient medical resources may not be able to screen and manage risk factors such as hypertension, hyperlipidemia, and diabetes mellitus in a timely manner, and the accessibility of related medications is also low, which leads to poor control of the TyG index and increased risk of stroke. Second, there was some heterogeneity among studies, which may be related to differences in study design, measurement methods, and stroke definitions: (1) Differences in the characteristics of the populations included in the studies (e.g. different geographic regions, age ranges, and genders) may have affected the results of the studies. (2) Smaller sample sizes or shorter follow-up times may lead to biased results or fail to accurately reflect the real situation. In this meta-analysis, although several studies were included, the sample size and follow-up time varied between studies, which is an important reason for the heterogeneity of the results. (3) The confounders adjusted for by the included studies were not all consistent, and residual confounders such as participants’ comorbidities, concomitant medications, and diet may have influenced the results despite the inclusion of studies analyzed multivariately. For example, the use of medications such as statins, antihypertensives, and hypoglycemic agents, which are commonly used to control cardiovascular risk factors, has the potential to alter stroke risk independently of TyG and its associated parameters. A systematic review and meta-analysis demonstrated that pre-stroke use of metformin was significantly associated with reduced mortality and improved functional outcomes [40]. This suggests that the TyG index may serve as a biomarker for identifying patients at high risk who may benefit from drugs that improve metabolic control, such as metformin. Therefore, the interaction of TyG index with antidiabetic drugs and the potential application of TyG index in guiding individualized treatment strategies should be further explored in future studies. By screening for the TyG index, physicians can identify high-risk patients more accurately and treat them with more aggressive metabolic control and therapy, thereby reducing the risk of stroke and improving prognosis. Additionally, chronic inflammation, which is closely associated with IR and atherosclerosis, may also be a confounding factor [41]. (4)While the formula for calculating the TyG index remains consistent across studies, differences in triglyceride and fasting glucose testing methods, reagents and instruments may affect its accuracy. (5) There are differences in the definition of stroke in different studies. For example, the study by Xia et al. (2024) exclusively included ischemic stroke patients, whereas other studies encompassed both hemorrhagic stroke or all stroke subtypes. Third, the TyG and its associated parameters are simple, inexpensive, suitable for mass screening, and associated with metabolic disease risk, with the potential to be integrated into risk assessment tools to improve stroke prediction. However, the optimal threshold values of TyG and its related parameters for predicting stroke risk are unknown. A dose-response analysis of 19 cohort studies by Yan et al. demonstrated that an increase of 1 mg/dl in the TyG index was associated with a 1.19-fold increase in the risk of cerebrovascular disease, thereby highlighting its clinical value as a continuous risk indicator [42]. A study of the Chinese population suggested that a TyG index > 8.81 in men and > 8.73 in women may indicate insulin resistance [43]. A study based on the China Health and Retirement Longitudinal Study (CHART) suggested that the critical value of the risk of all-cause mortality for TyG was 9.75, and a special analysis of patients with hypertension lowered the threshold of all-cause mortality to 9.45, reflecting that comorbidity has a moderating effect on the assessment of risk [44]. The NHANES cohort demonstrated a TyG threshold of 9.52 for cardiovascular mortality risk in hypertensive patients [45]. However, the TyG-BMI threshold increased to 269 in critically ill patients with respiratory failure [46], indicating a substantial modifying effect of disease severity on metabolic indicators. Consequently, future studies should investigate the potential impact of confounding factors such as race and region, medications, and inflammation, and ascertain the optimal critical value to enhance their predictive efficacy for stroke.