Kassanjee R, Johnson LF, Zaniewski E, Ballif M, Christ B, Yiannoutsos CT, et al. Global HIV mortality trends among children on antiretroviral treatment corrected for under-reported deaths: an updated analysis of the International epidemiology Databases to Evaluate AIDS collaboration. J Int AIDS Soc. 2021;24(Suppl 5):e25780.
Slogrove AL, Mahy M, Armstrong A, Davies MA. Living and dying to be counted: what we know about the epidemiology of the global adolescent HIV epidemic. J Int AIDS Soc. 2017;20:21520.
Ritchwood TD, Bishu KG, Egede LE. Trends in healthcare expenditure among people living with HIV/AIDS in the United States: evidence from 10 years of nationally representative data. Int J Equity Health. 2017;16:188.
Scott J, Agarwala A, Baker-Smith CM, Feinstein MJ, Jakubowski K, Kaar J, et al. Cardiovascular health in the transition from adolescence to emerging adulthood: a scientific statement from the American Heart Association. J Am Heart Assoc. 2025;14:e039239.
Shah ASV, Stelzle D, Lee KK, Beck EJ, Alam S, Clifford S, et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV: systematic review and meta-analysis. Circulation. 2018;138:1100–12.
Smit M, Brinkman K, Geerlings S, Smit C, Thyagarajan K, Sighem A, et al. cohort Ao: Future challenges for clinical care of an ageing population infected with HIV: a modelling study. Lancet Infect Dis. 2015;15:810–8.
So-Armah K, Benjamin LA, Bloomfield GS, Feinstein MJ, Hsue P, Njuguna B, et al. HIV and cardiovascular disease. Lancet HIV. 2020;7:e279–e293.
Zhu S, Wang W, He J, Duan W, Ma X, Guan H, et al. Higher cardiovascular disease risks in people living with HIV: a systematic review and meta-analysis. J Glob Health. 2024;14:04078.
Currier JS. Management of long-term complications of HIV disease: focus on cardiovascular disease. Top Antivir Med. 2018;25:133–7.
Papantoniou E, Arvanitakis K, Markakis K, Papadakos SP, Tsachouridou O, Popovic DS, Germanidis G, Koufakis T, Kotsa K: Pathophysiology and Clinical Management of Dyslipidemia in People Living with HIV: Sailing through Rough Seas. Life (Basel). 2024; 14.
van Wijk JP, Cabezas MC. Hypertriglyceridemia, Metabolic Syndrome, and Cardiovascular Disease in HIV-Infected Patients: Effects of Antiretroviral Therapy and Adipose Tissue Distribution. Int J Vasc Med. 2012;2012:201027.
Bosho DD, Dube L, Mega TA, Adare DA, Tesfaye MG, Eshetie TC. Prevalence and predictors of metabolic syndrome among people living with human immunodeficiency virus (PLWHIV). Diabetol Metab Syndr. 2018;10:10.
Arrive E, Viard JP, Salanave B, Dollfus C, Matheron S, Reliquet V, et al. Metabolic risk factors in young adults infected with HIV since childhood compared with the general population. PLoS One. 2018;13:e0206745.
Phuphuakrat A, Nimitphong H, Reutrakul S, Sungkanuparph S. Prediabetes among HIV-infected individuals receiving antiretroviral therapy: prevalence, diagnostic tests, and associated factors. AIDS Res Ther. 2020;17:25.
Daultrey H, Youseff E, Wright J, Davies K, Chakera AJ, Levett T. The investigation of diabetes in people living with HIV: a systematic review. Diabet Med. 2021;38:e14454.
Mellin J, Le Prevost M, Kenny J, Sturgeon K, Thompson LC, Foster C, et al. Arterial stiffness in a cohort of young people living with perinatal HIV and HIV negative young people in England. Front Cardiovasc Med. 2022;9:821568.
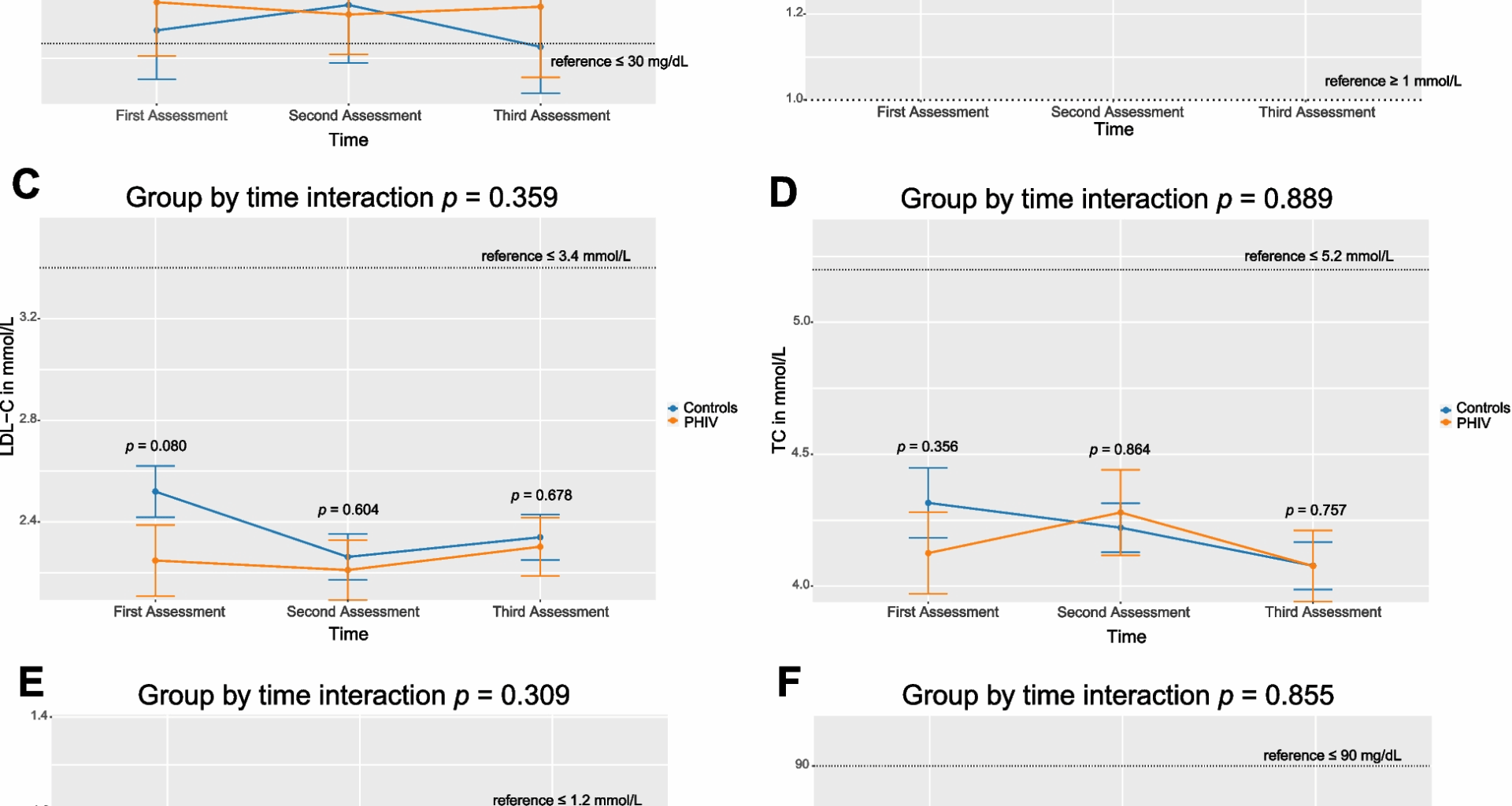
Davies C, Vaida F, Otwombe K, Cotton MF, Browne S, Innes S. Longitudinal comparison of insulin resistance and dyslipidemia in children with and without perinatal HIV infection in South Africa. AIDS. 2023;37:523–33.
Lopez E, Sainz T, Dirajlal-Fargo S, Jao J, Pinto J, Buchanan AM, et al. Cardiometabolic health burden in pediatric HIV: unmet need in the contemporary antiretroviral therapy era. Cureus. 2025;17:e85329.
Augustemak de Lima LR. Petroski EL, Moreno YMF, Silva DAS, Trindade E, Carvalho AP, Back IC: Dyslipidemia, chronic inflammation, and subclinical atherosclerosis in children and adolescents infected with HIV: The PositHIVe Health Study. PLoS One. 2018;13:e0190785.
Aurpibul L, Namwongprom S, Sudjaritruk T, Ounjaijean S. Metabolic syndrome, biochemical markers, and body composition in youth living with perinatal HIV infection on antiretroviral treatment. PLoS ONE. 2020;15:e0230707.
Irira ME, Philemon RN, Mmbaga JY, Komba V, Bartlett J, Kinabo GD, et al. Dyslipidemia in HIV-infected children and adolescents on antiretroviral therapy receiving care at Kilimanjaro Christian Medical Centre in Tanzania: a cross-sectional study. Infect Dis (Auckl). 2020;13:1178633720948860.
Carter RJ, Wiener J, Abrams EJ, Farley J, Nesheim S, Palumbo P, et al. Perinatal ACTS-HIVF-uaPEG: Dyslipidemia among perinatally HIV-infected children enrolled in the PACTS-HOPE cohort, 1999–2004: a longitudinal analysis. J Acquir Immune Defic Syndr. 2006;41:453–60.
Ayanful-Torgby R, Shabanova V, Essuman AA, Boafo E, Amoah LE, Paintsil E. Alterations in lipid profiles in children with perinatally acquired HIV infection living in Ghana: a cross-sectional study. PLoS One. 2025;20:e0318314.
Tune JD, Goodwill AG, Sassoon DJ, Mather KJ. Cardiovascular consequences of metabolic syndrome. Transl Res. 2017;183:57–70.
Li X, Zhai Y, Zhao J, He H, Li Y, Liu Y, et al. Impact of metabolic syndrome and it’s components on prognosis in patients with cardiovascular diseases: a meta-analysis. Front Cardiovasc Med. 2021;8:704145.
Wan H, Wu H, Wei Y, Wang S, Ji Y. Novel lipid profiles and atherosclerotic cardiovascular disease risk: insights from a latent profile analysis. Lipids Health Dis. 2025;24:71.
Rao SV, O’Donoghue ML, Ruel M, Rab T, Tamis-Holland JE, Alexander JH, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025;151:e771–862.
Kronenberg F, Mora S, Stroes ESG, Ference BA, Arsenault BJ, Berglund L, et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement. Eur Heart J. 2022;43:3925–46.
Vinci P, Di Girolamo FG, Panizon E, Tosoni LM, Cerrato C, Pellicori F, et al. Lipoprotein(a) as a risk factor for cardiovascular diseases: pathophysiology and treatment perspectives. Int J Environ Res Public Health. 2023. https://doi.org/10.3390/ijerph20186721.
Nguyen KA, Peer N, de Villiers A, Mukasa B, Matsha TE, Mills EJ, et al. Glycated haemoglobin threshold for dysglycaemia screening, and application to metabolic syndrome diagnosis in HIV-infected Africans. PLoS One. 2019;14:e0211483.
Daultrey H, Oliver NS, Wright J, Levett TJ, Chakera AJ. What is the influence of HIV serostatus on HbA1c? A prospective analysis using continuous glucose monitoring. Diabetes Care. 2024;47:1379–85.
Ulloque-Badaracco JR, Al-Kassab-Cordova A, Hernandez-Bustamante EA, Alarcon-Braga EA, Huayta-Cortez M, Carballo-Tello XL, et al. Association of apolipoproteins and lipoprotein(a) with metabolic syndrome: a systematic review and meta-analysis. Lipids Health Dis. 2023;22:98.
Behbodikhah J, Ahmed S, Elyasi A, Kasselman LJ, De Leon J, Glass AD, et al. Apolipoprotein B and cardiovascular disease: biomarker and potential therapeutic target. Metabolites. 2021. https://doi.org/10.3390/metabo11100690.
de Carvalho EH. Miranda Filho Dde B, Ximenes RA, de Albuquerque Mde F, de Melo HR, Gelenske T, Medeiros Zde B, Montarroyos U, Bandeira F: Prevalence of hyperapolipoprotein B and associations with other cardiovascular risk factors among human immunodeficiency virus-infected patients in Pernambuco. Brazil Metab Syndr Relat Disord. 2010;8:403–10.
Syed SS, Balluz RS, Kabagambe EK, Meyer WA 3rd, Lukas S, Wilson CM, et al. Assessment of biomarkers of cardiovascular risk among HIV type 1-infected adolescents: role of soluble vascular cell adhesion molecule as an early indicator of endothelial inflammation. AIDS Res Hum Retroviruses. 2013;29(3):493–500.
Van den Hof M, Klein Haneveld MJ, Blokhuis C, Scherpbier HJ, Jansen HPG, Kootstra NA, Dallinga-Thie GM, Van Deventer SJH, Tsimikas S, Pajkrt D, group Ns: Elevated Lipoprotein(a) in Perinatally HIV-Infected Children Compared With Healthy Ethnicity-Matched Controls. Open Forum Infect Dis. 2019; 6:ofz301.
van Genderen JG, Van den Hof M, de Boer CG, Jansen HPG, van Deventer SJH, Tsimikas S, Witztum JL, Kastelein JJP, Pajkrt D: Longitudinal Assessment of Lipoprotein(a) Levels in Perinatally HIV-Infected Children and Adolescents. Viruses. 2021; 13.
Van den Hof M, Ter Haar AM, Scherpbier HJ, Reiss P, Wit F, Oostrom KJ, et al. Lower IQ and poorer cognitive profiles in treated perinatally HIV-infected children is irrespective of having a background of international adoption. PLoS One. 2019;14:e0224930.
Van den Hof M, Ter Haar AM, Scherpbier HJ, van der Lee JH, Reiss P, Wit F, et al. Neurocognitive Development in Perinatally Human Immunodeficiency Virus-infected Adolescents on Long-term Treatment, Compared to Healthy Matched Controls: A Longitudinal Study. Clin Infect Dis. 2020;70:1364–71.
Van den Hof M, Jellema PEJ, Ter Haar AM, Scherpbier HJ, Schrantee A, Kaiser A, et al. Normal structural brain development in adolescents treated for perinatally acquired HIV: a longitudinal imaging study. AIDS. 2021;35:1221–8.
Cohen S, Caan MW, Mutsaerts HJ, Scherpbier HJ, Kuijpers TW, Reiss P, et al. Cerebral injury in perinatally HIV-infected children compared to matched healthy controls. Neurology. 2016;86:19–27.
Cohen S, Ter Stege JA, Geurtsen GJ, Scherpbier HJ, Kuijpers TW, Reiss P, et al. Poorer cognitive performance in perinatally HIV-infected children versus healthy socioeconomically matched controls. Clin Infect Dis. 2015;60:1111–9.
Statistics Uif: International Standard Classification of Education: ISCED 2011. pp. 84. Montreal; 2012:84.
WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development [https://www.who.int/tools/child-growth-standards/standards]. Accessed 4 Aug 2025.]
Age-based Pediatric Growth Reference Charts [http://www.bcm.edu/bodycomplab/BMIapp/BMI-calculator-kids.html]. Accessed 4 Aug 2025.]
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Khera AV, Everett BM, Caulfield MP, Hantash FM, Wohlgemuth J, Ridker PM, et al. Lipoprotein(a) concentrations, rosuvastatin therapy, and residual vascular risk: an analysis from the JUPITER trial (justification for the use of statins in prevention: an intervention trial evaluating rosuvastatin). Circulation. 2014;129:635–42.
Sainani KL. Dealing with missing data. PM&R. 2015;7:990–4.
Alberti KG, Zimmet P, Shaw J, Group IDFETFC. The metabolic syndrome–a new worldwide definition. Lancet. 2005;366:1059–62.
International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. Brussels: International Diabetes Federation; 2006. Available from: https://idf.org/media/uploads/2023/05/attachments-30.pdf. Accessed 2025 Jun 10.
Grundy SM. Metabolic syndrome scientific statement by the American Heart Association and the National Heart, Lung, and Blood Institute. Arterioscler Thromb Vasc Biol. 2005;25:2243–4.
Mehta A, Jain V, Saeed A, Saseen JJ, Gulati M, Ballantyne CM, et al. Lipoprotein(a) and ethnicities. Atherosclerosis. 2022;349:42–52.
Kikuchi DS, Kwapong YA, Schar M, Weiss RG, Sun K, Brown TT, et al. Lipoprotein(a) Is Elevated and Inversely Related to Coronary Endothelial Function in People With HIV. J Am Heart Assoc. 2024;13:e035975.
Appiah LT, Sarfo FS, Nguah SB, Huffman MD, Stiles JK, Feinstein MJ. Lipoprotein(a) and high sensitivity C-reactive protein among patients with HIV in Ghana: the study on cardiovascular risk profile of HIV-infected patients on HAART (SCRIPT). Glob Heart. 2020;15:74.
Mauss S, Berger F, Schmutz G, Henke J, Richter WO. Lipoprotein(a) in patients initiating antiretroviral therapy. HIV Med. 2008;9:415–20.
Enkhmaa B, Anuurad E, Zhang W, Abbuthalha A, Li XD, Dotterweich W, et al. HIV disease activity as a modulator of lipoprotein(a) and allele-specific apolipoprotein(a) levels. Arterioscler Thromb Vasc Biol. 2013;33:387–92.
Sprinz E, Lazzaretti RK, Kuhmmer R, Ribeiro JP. Dyslipidemia in HIV-infected individuals. Braz J Infect Dis. 2010;14:575–88.
Sainz T, Diaz L, Navarro ML, Rojo P, Blazquez D, Ramos JT, et al. Cardiovascular biomarkers in vertically HIV-infected children without metabolic abnormalities. Atherosclerosis. 2014;233:410–4.
Strehlau R, Coovadia A, Abrams EJ, Martens L, Arpadi S, Meyers T, et al. Lipid profiles in young HIV-infected children initiating and changing antiretroviral therapy. J Acquir Immune Defic Syndr. 2012;60:369–76.
Eissa MA, Mihalopoulos NL, Holubkov R, Dai S, Labarthe DR. Changes in fasting lipids during puberty. J Pediatr. 2016;170:199–205.
DeBoer MD. Assessing and managing the metabolic syndrome in children and adolescents. Nutrients. 2019. https://doi.org/10.3390/nu11081788.
Oselka N, Dubnov-Raz G, Ziv-Baran T. Using weight-for-age as a screening tool for metabolic syndrome in apparently healthy adolescents. Pediatr Res. 2025;97:994–1000.
Diaz-Ortega JL, Yupari-Azabache IL, Caballero Vidal JA, Conde-Parada NE, Rojas Gamboa AF. Criteria in the diagnosis of metabolic syndrome in children: a scoping review. Diabetes Metab Syndr Obes. 2023;16:3489–500.
Dzobo KE, Kraaijenhof JM, Stroes ESG, Nurmohamed NS, Kroon J. Lipoprotein(a): an underestimated inflammatory mastermind. Atherosclerosis. 2022;349:101–9.
Saumoy M, Sanchez-Quesada JL, Ordonez-Llanos J, Podzamczer D. Do all integrase strand transfer inhibitors have the same lipid profile? Review of randomised controlled trials in naive and switch scenarios in HIV-infected patients. J Clin Med. 2021. https://doi.org/10.3390/jcm10163456.
Neesgaard B, Greenberg L, Miro JM, Grabmeier-Pfistershammer K, Wandeler G, Smith C, et al. Associations between integrase strand-transfer inhibitors and cardiovascular disease in people living with HIV: a multicentre prospective study from the RESPOND cohort consortium. Lancet HIV. 2022;9:e474–85.
Friis-Moller N, Ryom L, Smith C, Weber R, Reiss P, Dabis F, et al. An updated prediction model of the global risk of cardiovascular disease in HIV-positive persons: The Data-collection on Adverse Effects of Anti-HIV Drugs (D:A:D) study. Eur J Prev Cardiol. 2016;23:214–23.
U.S. Department of Health and Human Services. Statin therapy in people with HIV. Adult and adolescent antiretroviral guidelines; 2024. Available from: https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-arv/statin-therapy-people-hiv. Accessed 2025 Jun 10.
Melvin AJ, Montepiedra G, Aaron L, Meyer WA 3rd, Spiegel HM, Borkowsky W, et al. Safety and Efficacy of Atorvastatin in Human Immunodeficiency Virus-infected Children, Adolescents and Young Adults With Hyperlipidemia. Pediatr Infect Dis J. 2017;36:53–60.
Nordestgaard BG, Langsted A, Mora S, Kolovou G, Baum H, Bruckert E, et al. Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications including flagging at desirable concentration cutpoints-a joint consensus statement from the European Atherosclerosis Society and European Federation of Clinical Chemistry and Laboratory Medicine. Clin Chem. 2016;62:930–46.
Darras P, Mattman A, Francis GA. Nonfasting lipid testing: the new standard for cardiovascular risk assessment. CMAJ. 2018;190:E1317–8.