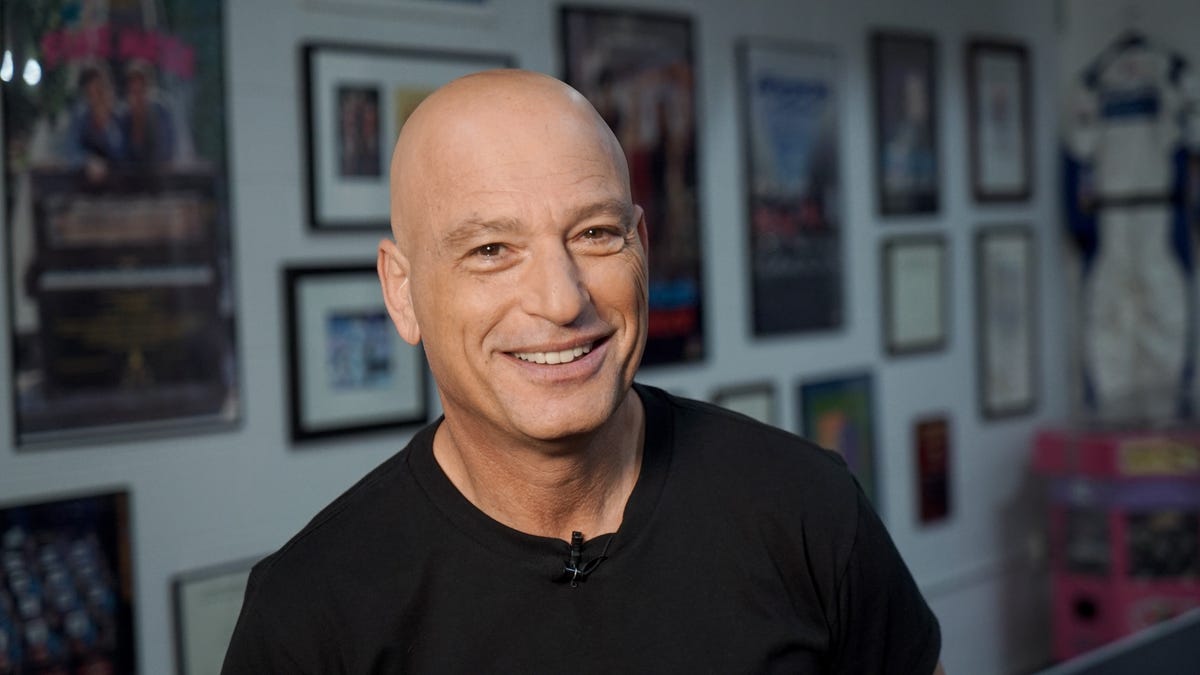
Howie Mandel talks ‘AGT’ sexiness, live-show vibe from makeup chair
During a pre-show makeup session in his dressing room, “AGT” judge Howie Mandel explains performer pressure, crew precision on the day of a live show.
Dan MacMedan, USA TODAY
Howie Mandel wasn’t diagnosed with obsessive-compulsive disorder (OCD) until his 40s, but he says the condition profoundly impacted his entire life.
“I don’t remember not experiencing OCD,” the “America’s Got Talent” judge says over the phone, just two days after his 70th birthday.
Obsessive-compulsive disorder affects an estimated 1.2% of U.S. adults, and OCD sufferers usually go undiagnosed for 10 or more years. Mandel says the condition is deeply misunderstood — his symptoms, which he calls debilitating, stretch far beyond “germaphobe” stereotypes.
“I can’t tell you how many people in the course of a week will come up to me and say, ‘I have a little bit of that.’ Well, you don’t have a little bit of OCD,” he says.
The comedian has been a partner of NOCD, a company that provides video-based OCD therapy, since 2022. Now more than ever, Mandel recognizes the need for accessible, reliable mental health care, especially with the growing concerns around “AI therapy.”
Mandel has become a strong advocate for seeking mental health support, but his own journey wasn’t easy.
‘I can’t show up, and my life stops’
People with OCD may experience uncontrollable and recurring thoughts (obsessions), engage in repetitive behaviors (compulsions), or both. These obsessions and compulsions can vary from person to person. Some people couldn’t care less about dirt and germs, but are fixated on “bad things” happening to people they love and care about.
“People interpret OCD as being persnickety or being really neat or fastidious, that is not OCD,” he explains. “OCD is a nightmare if you are diagnosed with it… and a lot of people have it and are misdiagnosed.”
Mandel still has people insist their hands aren’t dirty; that he can shake them. But what those people don’t understand is that it’s not as simple as just shaking hands.
“For me, it’s about getting triggered into thinking there’s something on my hand, and then being stuck at a sink, scalding my hand for the next 12 hours,” he explains. “Not being able to carry on life (as a) husband, father and provider. I can’t show up, and my life stops. I’m in this nightmare where I think terrible things are going to happen.”
Intellectually, he knows these terrible things will not occur. But that makes it even more horrific, he says, because he can’t control his dark thoughts. Or, he is compelled to do a ritual to quell them: “It drives you nuts, and you can’t function. It’s debilitating.”
Telehealth helps rural communities access mental health care
On “America’s Got Talent” (AGT), contestants tell Mandel that a roadblock stopped them from achieving their hopes and dreams.
“But I think the biggest predicament that we all share is mental health,” Mandel says.
The U.S. is in a rural mental health crisis; 65% of rural counties do not have a psychiatrist, according to Mental Health America. Research shows that treatment accessibility, availability, stigma and both geographical and social isolation contribute to higher suicide rates in rural areas compared to urban areas. The risk of suicidal ideation is also significantly higher among those with OCD compared to the general population.
AI tools like ChatGPT are increasingly used for therapy, but the results can be problematic. Mental health experts warn that using AI tools as a replacement for mental health support can be particularly dangerous for people grappling with OCD, or similar conditions.
While AI is accessible, Mandel doesn’t see that as the answer — it would be like telling someone with appendicitis to go on WebMD, he says.
“If you really feel like you are suffering, AI isn’t the answer,” Mandel says. “That is not a tool for mental health, just like it’s not a tool for physical health.”
Mandel hopes that one day, an AI chatbot like ChatGPT would refer users showing signs of OCD to NOCD, where they can speak to a real-life therapist with expert training in OCD and exposure and response prevention (ERP) therapy.
He says that telehealth services like NOCD can be a game-changer for OCD treatment, particularly for people living in middle America. (Though rural residents often lack insurance coverage, NOCD does accept most insurance plans.)
“For OCD, you have to go to someone who is an expert… not only an expert in therapy for it, but an expert for diagnosing it,” he says. If someone happens upon his story, he hopes they will arrange an appointment to at least get diagnosed. From there, they can find the right treatment plan to manage their symptoms.
“It’s a constant journey, and it’s a constant battle that I, for the most part, am winning. But the battle goes on,” Mandel says. “It’s worth battling.”