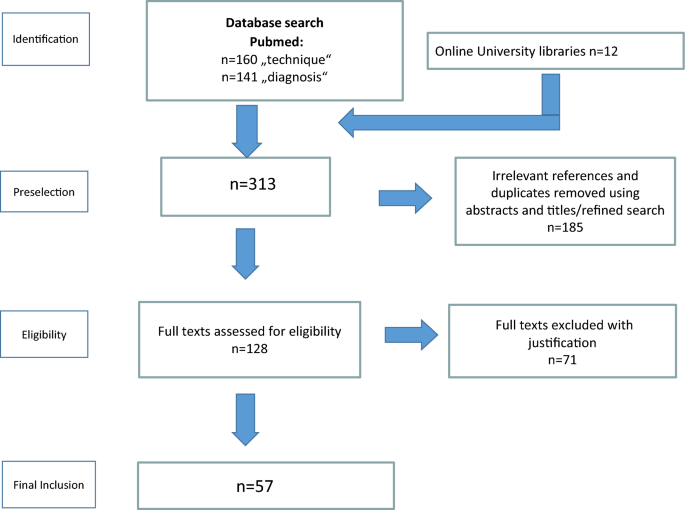
Literature search and study selection
An initial search using the search terms related to the operative technique yielded 160 records, the search related to the diagnostic tools yielded 141 records. In addition, 12 articles were found by further examining the reference lists of the originally identified publications.
185 articles were removed as irrelevant to the stated research question or were duplicates. Of all 313 relevant publications, a total of 57 articles remained after the precise evaluation (Fig. 1).
Flow chart of the study selection process
The majority of publications were from the USA, followed by the Netherlands and United Kingdom. The extracted data included information on surgical procedures, diagnostic methods, patient-specific characteristics and outcomes.
After the literature had been completely reviewed, it was tabulated including the year of publication, first author, country of origin, type of study, diagnostic or surgical technique.
Diagnosis technology
The diagnosis of craniosynostosis has been the subject of 19 studies, many of which yield overlapping findings that allow for a concise summary of key diagnostic methods (Table 1). This section highlights significant advancements and insights from pivotal studies, showcasing how these approaches have shaped current diagnostic strategies.
Table 1 Literature diagnostics of sagittal suture CSO
In 2003, Cedzich and Farmand published the status of the necessary diagnosis of craniosynostosis. Accordingly, an existing suspected diagnosis should be confirmed at that time by a posterior-anterior and a lateral conventional X-Ray of the skull and a more detailed image should also be obtained by computed tomography (CT). A scintigraphy image (SPECT) of the occluded suture was also taken to be able to assess a possible final occlusion based on the basis of reduced activity. Sonographic imaging was only recommended for follow-up purposes [26].
The study by Agrawal et al. in 2006 analysed 114 children with isolated sagittal synostosis to assess if clinical diagnosis alone suffices for surgery. In most cases, the clinical findings were consistent with surgical and histopathological outcomes. Pathological examinations were performed in 104 of 114 children, all of which confirmed the diagnosis of sagittal craniosynostosis. Radiological investigations were often unnecessary, reducing radiation exposure and healthcare costs. The study concluded that surgery could proceed based on clinical diagnosis when symptoms are typical [27].
Marcus et al. introduced Mid-Sagittal Vector Analysis (MSVA) as a CT-based morphometric technique to assess cranial morphology in sagittal craniosynostosis in 2006. Pre- and postoperative CT scans of 16 patients were analysed, identifying three key affected regions: frontal, vertex, and occipital. MSVA effectively quantified preoperative deformity and postoperative correction. Uniquely, this method provided an objective, region-specific, and quantifiable assessment of cranial shape changes, offering a more precise evaluation of surgical outcomes compared to traditional qualitative assessments [28].
In their study of 67 patients with isolated craniosynostosis, Fearon et al. in 2007 demonstrated that CT imaging is unnecessary due to the condition’s clear clinical detectability and the associated risk of radiation exposure. In 66 of 67 children, the findings of the clinical and radiological examinations were similar in their description and associated diagnosis. Only one child with suspected lambdoid synostosis was radiologically diagnosed with positional plagiocephalus. In addition, 3/4 of the craniofacial surgeons rated CT as unnecessary for surgical intervention. Fearon et al. advise that due to the associated risks, including the need for additional sedation in children, and the significant cost of this procedure, CT scans should be reserved for cases where craniosynostosis cannot be clearly diagnosed by clinical assessment [29].
Wilkie et al. (2010) analysed 326 children with craniosynostosis (144 non-syndromic, 44.5% sagittal synostosis) who underwent genetic testing. Results showed that 21% of all non-syndromic had a genetic cause, mainly single-gene mutations (86%) and fewer chromosomal abnormalities (14%) with the FGFR3 P250R mutation being the most common. Coronal synostosis had the highest genetic association. In contrast, sagittal craniosynostosis showed minimal genetic links, with only a small percentage linked to single-gene mutations and even fewer chromosomal abnormalities. This suggests non-genetic factors play a greater role in sagittal craniosynostosis, though further research is needed. It provides valuable insights into surgical prognosis, recurrence risk, and informs the development of future surgical strategies [30].
In 2011 Ciurea et al. described the current state of diagnostics and therapy and emphasized the 3D CT scan as the preferred diagnostic method for the detection of scaphocephaly. Due to the radiation exposure caused by conservative X-ray diagnostics, this procedure was not recommended. Clinical examination methods such as head circumference or sonography were indicated as being of inferior importance [31].
As a pioneering new alternative to conventional CT imaging, Eley et al. (2014) examined the so-called “black bone MRI” (in 2D and 3D). A total of 13 children suffering from craniosynostosis underwent this new examination method and the results were compared with standard CT scans. Within a “black bone image”, physiological sutures contrast from the cranial bones with increased signal intensity, prematurely closed ones do not, so the clinical potential for diagnosis without radiation became evident [32]. Classic MRI was still recommended if there is clinical evidence of an intracranial anomaly [3, 4, 33].
In 2015, Rozovsky et al. investigated the utility of cranial ultrasound (CUS) as a first-line imaging modality for diagnosing craniosynostosis in infants under 12 months, benchmarking its diagnostic accuracy against radiography. Their study revealed complete concordance between CUS and radiography in assessing especially the sagittal sutures. Overall, the results demonstrated that CUS possesses high sensitivity (100%) and specificity (98%), reliably detecting suture abnormalities while eliminating the risks associated with ionising radiation. These findings underscore the value of CUS as a safer, non-invasive alternative to radiography, particularly for initial assessments [34, 35].
Fearon et al. examined in 2017 a total of 392 craniosynostosis patients to validate the CI method, which is calculated by multiplying the maximum skull width by 100 and dividing it by the skull length. They found no significant correlation between the measured CI and the subjectively assessed severity. In addition, they note that the CI method cannot capture certain postoperative changes, such as changes in occipital skull height after sagittal suture synostosis surgery, or accurately reflect the complexity of skull deformities [7].
Cornelissen et al. examined in 2018 whether prenatal ultrasound can help detect sagittal craniosynostosis scaphocephaly among others. Researchers analysed 20-week ultrasounds from 41 affected foetuses and 82 controls, focusing on skull measurements like biparietal diameter (BPD), occipitofrontal diameter (OFD), and the CI. Findings showed that foetuses with scaphocephaly had a significantly lower CI (0.76 vs. 0.79; p = 0.000), but CI alone was not reliable for screening at 20 weeks. However, a growth deviation in BPD from week 20 onward suggested that 3D imaging of cranial sutures may be beneficial in suspected cases [36].
In 2020 De Jong et al. investigated the use of 3D stereography as an alternative diagnostic method to CT examinations, as well as to supplement a possible lack of expertise. By capturing photographic images of the child’s head from different angles and merging them using special software, a precise three-dimensional individual model is created. In combination with a “deep learning algorithm”, this enabled the visualisation of deviations from the ideal form, whereby a comparison with a healthy cohort is applied. The accuracy of this method is clearly demonstrated by the exact classification of 195/196 cases (99.5%), with a sensitivity of 100% and a specificity of 96% for scaphocephaly [8].
In 2021 Ravindra et al. investigates the necessity of preoperative CT imaging in infants with yet clinically diagnosed single suture craniosynostosis, including sagittal craniosynostosis. The authors analysed whether CT findings confirmed the clinical diagnosis and influenced surgical decision-making. Results demonstrated that in most of the cases, CT imaging corroborated the clinical diagnosis and rarely altered the surgical approach. Consequently, the authors suggest that routine preoperative CT imaging may not be essential in cases with a clear clinical diagnosis, thereby potentially reducing radiation exposure in affected infants [37].
The study by Cinca et al. published in 2022, explores the potential role of mechanical constraints in the development of sagittal suture craniosynostosis in twin pregnancies. The study analyses prenatal ultrasound data and suggests that restricted space in the uterus could contribute to the early fusion of the sagittal suture, leading to an abnormal head shape. The authors propose that mechanical factors, such as crowding or abnormal positioning of the twins, may be a significant factor in the development of SSC, alongside genetic causes [38].
In the article published in 2023, Schmidt et al. explained that in sonography an echo-poor gap between the adjoining cranial bones can be recognised in an intact suture, which corresponds to the fibrous unclosed suture; in an ossified cranial suture, however, a corresponding gap is missing [2]. The sensitivity of this method is reported to be almost 100%, the specificity is 86–98% compared to the CT collective [2].
In addition to sonography, Schmidt et al. recommend in 2023 other, in some cases very classic, minimally invasive methods for confirming a possible suspected diagnosis of craniosynostosis during an initial clinical examination. The pathognomonic shape of the skull, viewed from the vertex, is usually the first thing that attracts attention. The sutures can then be palpated; a hardened (osseous) palpable thickening would be noticeable. Another recommended method of assessment would be to determine the CI. This parameter is particularly appropriate for the presence of scaphocephaly and for follow-up assessment, even after surgery [2].
Surgical perspectives
38 studies have investigated surgical therapies for craniosynostosis, with many reporting overlapping findings. These studies largely agree on the efficacy and limitations of various techniques, highlighting the importance of age, method, and postoperative care in achieving optimal outcomes. Below, key studies and their findings are summarised to provide an overview of therapeutic advancements (Table 2).
Table 2 Surgical techniques
The Pi procedure, introduced by Jane et al. in 1978 and named after the Greek letter π, involves dynamic cranioplasty using osteotomies shaped like the symbol π to enable controlled cranial expansion [39]. Unlike total cranial vault remodeling, the procedure preserves the sagittal suture and reshapes the skull with bone strip removal and compression [39, 40]. Magge et al. noted no significant reduction in surgical burden compared to endoscopic craniectomy, though its long-term benefits remain debated [41]. In a 20-year retrospective analysis of open cranial vault repairs, Morrison et al. focused on reoperation and complication rates, emphasising that despite the historical importance of open techniques like these, they do not necessarily reduce complications or the need for additional surgeries [42]. Their studies underscore the ongoing challenges in achieving optimal long-term outcomes and the importance of evaluating reoperation rates and exploring alternative approaches.
In the early 1990s, Maugans et al. compared the strip craniectomy (SC) method with the more extensive calvarial vault remodeling (CVR) procedure for the treatment of sagittal craniosynostosis to delay premature ossification. CVR is an invasive surgical technique for treating craniosynostosis by removing, reshaping, and repositioning parts of the skull. This procedure corrects skull deformities, allows for normal brain growth, and helps prevent increased intracranial pressure. In contrast to the CVR method, bone defects were found in 59% of the SC patients at the final examination, and two patients had to be operated once again due to suboptimal cosmetic results (with the CVR method). The results showed that the effectiveness of SC procedures decreases with increasing age, in contrast to the CVR method [43].
More studies on CVR for craniosynostosis, including work by Birgfeld et al. and Seruya et al., focus on surgical safety, outcomes, and suture patency. Birgfeld et al. emphasize the role of multidisciplinary teams in ensuring safe open cranial vault surgery. Seruya et al. retrospectively assessed cranial suture patency using postoperative CT scans taken approximately 6–12 months after total cranial vault remodeling for isolated sagittal synostosis. A neurosurgical consultant rated the bilateral coronal and lambdoid sutures based on axial and 3D-reconstructed imaging, assigning scores of 0 (closed), 1 (partially open), or 2 (fully open). Partial patency was defined by alternating open and fused segments across consecutive axial slices. Scores from the four sutures were summed to yield a total score between 0 and 8. Only repositioned vault regions were evaluated, with the basilar skull excluded. This structured approach enabled consistent, quantifiable comparisons across patients and subgroups. Both highlight the effectiveness of CVR but stress the importance of surgical planning and postoperative monitoring [44, 45].
Panchal et al. (1999), examined 40 infants with sagittal craniosynostosis to determine whether the postoperative outcome in relation to the cranial index can be linked to the child’s age and the extent of the operation. He concluded that, extended SC for sagittal craniosynostosis does not lead to a normal ratio between skull width and length, even if performed before 4 months of age. Nevertheless, performing subtotal calvariectomy (SCT) within the first 13 months of life typically restores a normal skull width-to-length ratio in most children [46].
Due to the persistently existing complication and revision rates of open surgical approaches, Jimenez & Barone developed an alternative method for treating craniosynostosis in 1998, based on four successfully performed operations. In addition to the removal of the premature suture, this technique also included the so-called Barrel-Staves osteotomies of the temporal and parietal bones [9]. Barrel-stave osteotomies are a surgical method to reshape bones, often used in craniosynostosis treatment. Multiple parallel bone cuts increase flexibility, allowing the bone to be reshaped and stabilised with plates or screws, ensuring structural integrity [47, 48]. They also used helmet therapy afterwards, initially for sagittal suture synostosis [1, 49]. An average operating time of 1.68 h with an average blood loss of 54.2 ml was determined. Three out of four patients did not require a blood transfusion and could be discharged after just 24 h. In a subsequent follow-up visit after eight to 15 months, the authors found that all patients had undergone successful and sustained correction of the scaphocephaly [9].
In their 2004 publication, the authors further explored endoscopically assisted wide vertex craniectomies combined with bitemporal and biparietal Barrel-Staves osteotomies for the treatment of 139 patients with sagittal synostosis. The patients were on average 3.6 months old. A total of 9% (two intraoperative, 12 postoperative) required blood transfusions, the mean blood loss was 29 ml. 120 out of 139 patients could be discharged on the following day. The results showed that 87% of patients had excellent outcomes with a cephalic index of over 75, 8.7% had good outcomes between 70 and 75 and 4.3% had poor outcomes (< 70) had poor outcomes. The mortality rate was lower than with traditional reconstruction methods such as full CVR, and no serious complications occurred [15].
One year later this group presented their 16 years of experience to date in treating a total of 256 patients with sagittal synostosis using the method described above. Blood loss was reduced to an average of 27 ml and the transfusion rate to 7%. Discharge was also possible after an average of one day. The very high success rate of 87% remained similar to subsequent years despite the change in CI guidelines (87% of patients achieved a CI above 80, 9% a CI of 80–70 as good and 4% < 70 as poor) [50].
Recent studies on endoscopic strip craniectomy (ESC) for craniosynostosis, including work by Lobb et al., Valetopoulou et al., Ahn and Bhandarkar and Magge et al. explore various aspects of the technique [41, 51,52,53,54]. Common themes include its effectiveness in treating sagittal and metopic synostosis, the use of helmet therapy post-surgery, and comparisons with other surgical approaches like spring-assisted cranioplasty. Differences include the focus on patient age, incision techniques, and long-term outcomes [41, 51,52,53]. Further contributing to this field, Riordan et al. conducted a longitudinal cohort study examining ESC for infantile craniosynostosis, demonstrating favourable outcomes for infants undergoing ESC [55]. Similarly, Gociman et al. explored minimally invasive strip craniectomy for sagittal synostosis in a retrospective study, providing evidence for the technique’s efficacy in treating this condition [56]. These studies, along with others, underscore the growing body of evidence supporting the use of ESC as a treatment for craniosynostosis, especially in younger patients.
Fearon et al. 2009 conducted in 2009 a retrospective analysis of children with nonsyndromic single sutural synostosis who underwent a single CVR procedure. The study found that while cranial indices normalised with low preoperative rates and minimal complications, post-surgical growth did not fully return to normal, with a tendency for the calvaria to revert towards the original deformity. The authors concluded that surgeons should aim for overcorrection rather than just normalisation of the skull shape, particularly in younger patients. This raised concerns about the effectiveness of endoscope-assisted procedures and postoperative molding. Furthermore, delaying surgery may improve long-term aesthetic outcomes, but the timing should carefully consider potential brain development risks and the need for full reconstruction in children over 10 months of age [57].
In 2011, Sha et al. investigated differences in the efficacy and morbidity of minimally invasive endoscopic wide vertex SC with the use of barrel-starves osteotomies and postoperative helmet orthosis for an average of 8.7 months compared to open cranial vault reconstruction for sagittal craniosynostosis. A total of 89 children were included, 47 underwent endoscopic surgery at an average age of 3.6 months and 42 underwent open surgery at an average age of 6.8 months. The endoscopic method not only showed a significantly lower mean blood loss (29 ml compared to 218 ml in the open method) and a lower transfusion rate (all openly operated children received one, whereas only 3 endoscopically operated children received one), but also allowed a significantly shorter postoperative hospitalisation (1.2 days compared to 3.9 days in open procedures). It is also noteworthy that the pre- and postoperative CI after 13 months were comparable in the endoscopically treated children (68% and 76%), while the open procedures had comparable CI values after 25 months (68% and 77%) [58].
In 2013, Van Veelen et al. investigated the outcome of extended SC on a total of 79 consecutive sagittal suture synostosis patients. Four OP—techniques were used: A–D, from simple bilateral parietal flap with breaking out the bone roof to remodeling the parietal flap by adding triangular incisions and bending or suturing. Compared to the initial CI, variant D, in which the excised sagittal strip is fixed rotationally between the parietal lobes, showed the greatest initial improvement. After two years of follow-up, however, no significant difference was found between the variants. The mean blood loss was 230 ml, and four patients had to undergo further surgery due to increased intracranial pressure [59].
In 2015, Van Veelen et al. compared the classic fronto-parietal reconstruction with a modified version of this technique, in which the removed bone piece is rotated by 90° and fixed between the parietal bones to increase the width of the skull. The study included 69 children diagnosed with sagittal suture synostosis. During the follow-up the head circumference decreased in both groups, whereby the preoperative head circumference had the decisive influence, but not the chosen surgical technique. Furthermore, aesthetic results and associated complications like the prevalence of headaches were found to be comparable in both groups. Both groups also showed a similar blood loss of 1174 ml in the classic group and 914 ml in the modified group. Van Veelen et al. concluded that the addition of a widening bridge in the context of late complete remodeling (older than 9 months) significantly and long-lastingly improves CI [60].
In a prospective multicenter registry study conducted by Lang et al. 2021, which included children between 2012 and 2019, the results of minimally invasive surgical methods, ESC versus spring-mediated cranioplasty (SMC) were compared. The study involved a total of 676 children, all under the age of 6 months, who were diagnosed with sagittal suture synostosis. Among them, 580 were ESC infants from 32 centres, and 96 were SMC infants from five centres. The results indicated no significant difference in the incidence of a transfusion-free hospital course between the two groups. However, the likelihood of being admitted to the intensive care unit, as well as the length of stay and the overall hospitalisation duration, was greater in the spring-assisted surgery group, potentially due to the hospital’s protocol [61]. Further supporting the efficacy of SMC, Rodriguez-Florez et al. demonstrated significant three-dimensional calvarial growth following this intervention, highlighting its potential in reshaping cranial morphology [62]. Similarly, Rodgers et al. analysed 100 consecutive cases of nonsyndromic scaphocephaly treated with SMC and confirmed positive outcomes, reinforcing its role as a viable alternative to ESC [63]. Additionally, Pyle provided a comprehensive surgical manual detailing the manufacturing and application of springs in craniofacial surgery, further contributing to the standardisation of this technique [64].