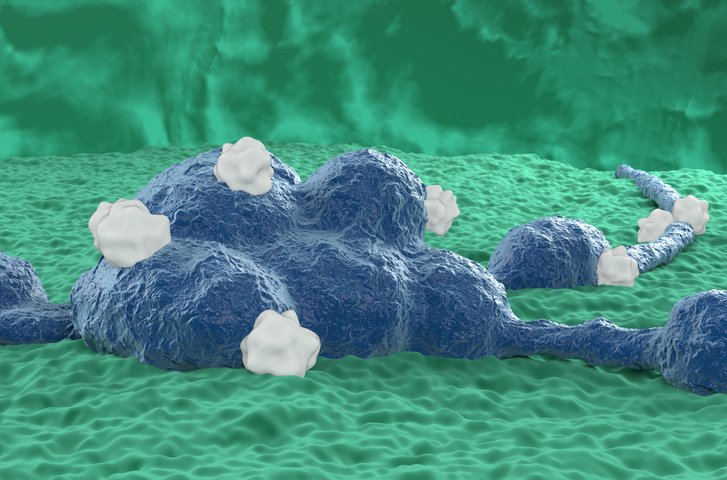
 Credit: Nemes Laszlo/Getty Images
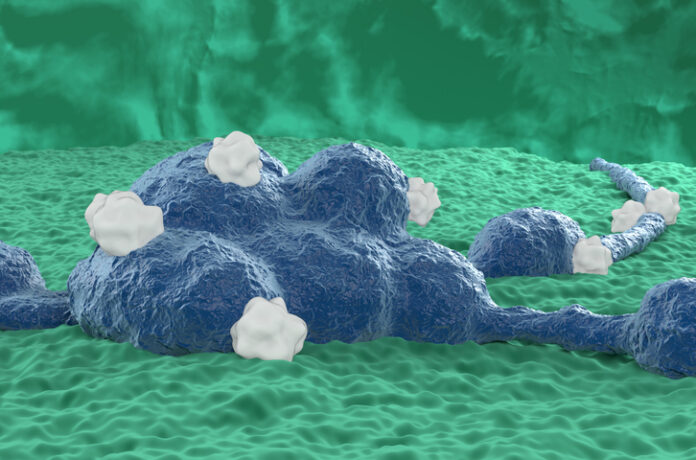
Credit: Nemes Laszlo/Getty Images
Researchers at St. Jude Children’s Research Hospital have reported encouraging results for a novel neuroblastoma immunotherapy that could address treatment resistance, a very common problem for this form of cancer. In a study published in Nature Communications, the research team reports how these tumors become resistant and developed a combination treatment that can effectively eliminate neuroblastoma and prevent relapse.
Neuroblastoma is a rare type of cancer impacting nerve tissue that primarily affects children under the age of five, often arising during fetal development driven by MYC oncogenes. The low number of mutations typically found in these tumors can severely limit the efficacy of immunotherapy approaches, such as checkpoint inhibitors, and the five-year survival rate for high-risk neuroblastomas remains lower than 50% with currently available treatments.
“While functional genomic screens have identified many essential survival genes in neuroblastoma cells, translating these discoveries into effective therapies has been technically challenging because most of these essential genes, including MYC, are considered to be ‘undruggable’,” stated the authors of the study, led by Jun J. Yang, PhD, professor of pharmacogenomics at St. Jude Children’s Research Hospital.
A previous study by Yang and colleagues had identified RBM39 as a promising drug target for neuroblastoma and other MYC-driven cancers. Indisulam, an experimental “molecular glue” drug that marks the RBM39 protein for proteasomal degradation showed high efficacy against high-risk models of neuroblastoma. However, the tumors eventually relapsed in most cases, which urged the researchers to investigate the mechanisms behind this resistance in order to overcome it.
Neuroblastoma cells typically present one of two major cellular states: adrenergic and mesenchymal. Previous research had suggested that these cells can switch from one state to another in response to treatment to gain resistance, as these cellular states respond differently to a variety of interventions including chemotherapy. However, how neuroblastoma cells switch states during treatment was still unknown.
“Our study addresses one key knowledge gap in therapy resistance: how cellular plasticity of cancer cells confers drug resistance in neuroblastoma,” wrote Yang and colleagues. “Addressing this question is a key step towards developing more effective combination therapies against refractory malignancies.”
Using RNA sequencing, the study created a transcriptomics and epigenetic map of high-risk neuroblastoma models, including human cells and patient-derived xenograft mice. Results showed that neuroblastoma cells in relapsed tumors could switch from an adrenergic to a mesenchymal state, and vice versa, by acquiring a transcriptional profile that resembled that of neural crest stem cells.
The study also found that neuroblastoma cells switching states had higher levels of the GD2 glycolipid, which is the target of dinutuximab, an FDA-approved immunotherapy for children with high-risk neuroblastoma. While anti-G2D antibodies like dinutuximab significantly improve survival, not all high-risk patients respond to this form of treatment. Based on these findings, the researchers hypothesized that a combination treatment consisting of indisulam would not just achieve high response rates, but also prevent relapse. In a mouse model of neuroblastoma, this combination resulted in the complete eradication of the tumors, achieving durable responses.
While more research will be needed to confirm these effects and initiate clinical trials, Yang and colleagues see potential for this approach beyond neuroblastoma, potentially benefiting patients with other cancer types typically treated with antibody immunotherapies.