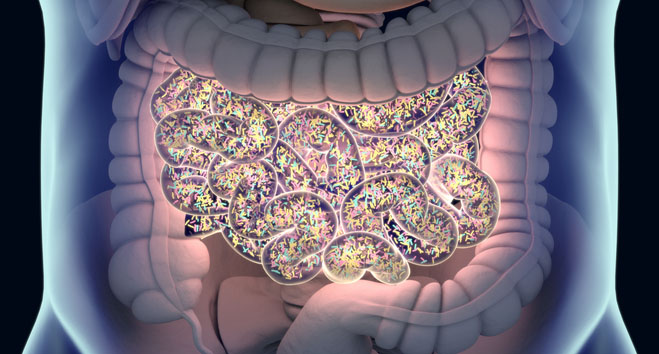
 Credit: ChrisChrisW/Getty Images
Credit: ChrisChrisW/Getty Images
Researchers from Novome Biotechnologies and Stanford University have reported encouraging clinical data from a novel approach to achieve stable gut colonization with a microbiome therapy for kidney stones. While their findings, published in Science, show promise to overcome a major challenge for microbial therapeutics, they also highlight efficacy and biosafety limitations that still need to be addressed in this emerging field.
Therapeutic approaches targeting the gut microbiome have been rapidly garnering attention in medical research due to the important role that the human microbiome plays across a myriad of physiological processes. However, many approaches to precision microbiome therapeutics have failed in clinical trials due to difficulties achieving long-term engraftment within the native gut flora.
“Despite showing efficacy in animals and a good safety profile in humans, these therapeutics have struggled to show clinical efficacy,” stated the researchers. “A colonizing strategy may enable therapeutic concentrations high enough to drive the activity necessary for efficacy.”
To overcome this long-standing challenge, the researchers designed a genetic engineering strategy that allowed them to control the colonization and removal of the microbiome therapy. In a previous study, Phocaeicola vulgatus, a common gut bacterium, was engineered to feed on porphyran, a nutrient found in seaweed, and to depend on its presence to express genes essential for their survival.
“We chose porphyran as a candidate for creating an exclusive niche for our engineered bacteria because only 2% of Western individuals appear to harbor a native porphyran-utilizing microbe,” stated the researchers. This provides an unoccupied ecological niche within the gut that the engineered bacteria can occupy without competing with native microbes.
In the current study, the bacteria were also engineered to include a five-gene module designed to break down oxalate, a compound that forms kidney stones. This strategy is intended to treat enteric hyperoxaluria, a condition that commonly arises as a side-effect of gastric bypass operations that results in high oxalate levels and recurring kidney stones.
In mice and healthy human volunteers, the treatment showed successful engraftment, with levels of bacteria varying according to the daily amount of porphyran taken by participants in their diet. “A single dose of the strain was sufficient for colonization if the subject was provided proper gastric protection, and even at high doses of porphyran, the treatment was safe and well tolerated,” reported the researchers. No serious adverse effects reported, as well as no discernible changes in the diversity of the native microbiota.
As expected, removing porphyran from the diet resulted in the elimination of the engineered bacteria in most of the subjects. However, four out of 19 participants who originally achieved engraftment still showed detectable levels of the bacteria after stopping the treatment. Genomic sequencing revealed that this was caused by either point mutations or genome rearrangements that allowed the essential genes to maintain expression independently of porphyran intake.
In the Phase IIa arm of the study, the treatment was tested in individuals with enteric hyperoxaluria following gastric bypass operations. In this population, engraftment was less consistent and abundant compared to the results seen in healthy volunteers, resulting in inconsistent efficacy results. While the treatment reduced oxalate levels by 47% in a rat model of enteric hyperoxaluria, only a statistically insignificant trend towards oxalate reduction was observed in humans.
Sequencing studies showed that these results were mainly due to horizontal gene transfer; in some cases, the engineered bacteria introduced new genes from their neighbors that replaced the oxalate pathway, while in others, native bacteria of the same family took up the genes to metabolize porphyran and started competing with the therapeutic strain.
Despite mixed results, the research team highlighted the early potential shown by this novel approach to achieve stable, long-term gut colonization with microbiome therapy. Future work into more robust systems to control colonization and elimination of therapeutic strains will help the development of more effective microbial treatments. Additionally, further research will be needed to investigate the significant differences observed between healthy volunteers and patients with enteric hyperoxaluria, which may be related to alterations in the gut microenvironment caused by the disease.
In future studies, the research team is considering replacing porphyran with a synthetic nutrient in hopes to create a more exclusive niche for the engineered therapy and make the treatment suitable for populations with higher seaweed consumption in their diet, which is the case across many regions of Asia.
