Patients and study design
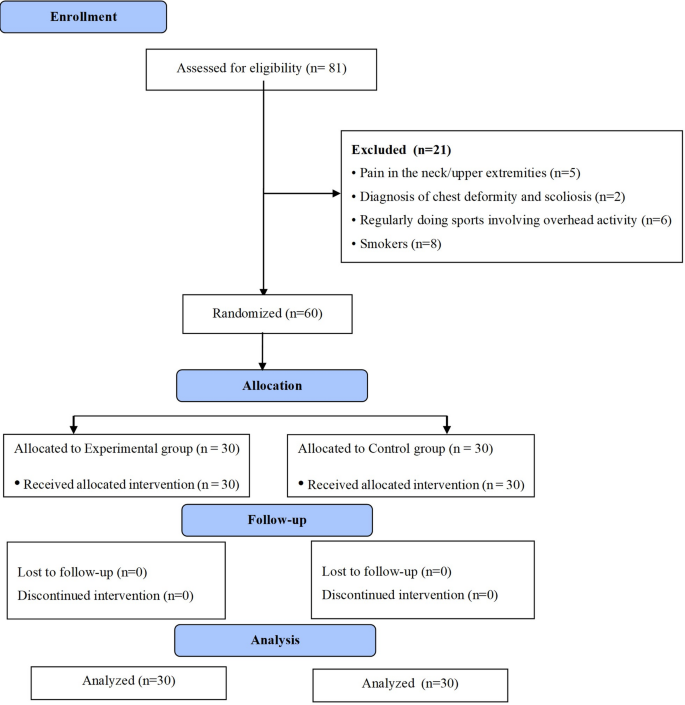
Between September 2017 and May 2019, 60 healthy university students from X University Campus participated in this prospective, two-arm, randomized controlled study conducted at X University, X Department. Because there were no relevant studies, a priori sample size calculation for ANOVA: repeated measures, time‒group interaction was performed via G*Power software using medium effect size “f ” as 0.25 (95% power, 5% Type-I error level). A sample size of 27 participants per group was determined, and we decided to include 30 participants in each group, with a 1:1 ratio, in case of dropouts (10%).
The primary author (SSY) screened participants for eligibility, generated the random allocation sequence, and assigned them into groups. A computer-generated list of random numbers was used to allocate (concealed by envelopes) the participants into the experimental group (EG) or control group (CG) (Fig. 1). The EG performed elbow flexion exercises with a BFR exercise set attached on the dominant side 3 times a week [1] for 6 weeks. The CG received no exercise but rather an informational brochure about exercise and injury prevention. Elbow and shoulder JPS, elbow flexion and extension strength, and upper extremity functional motor performance were measured on the dominant upper extremity in random order, at the beginning and after 6 weeks. Any learning effect was excluded by performing a previous familiarization session for all tests.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram of the study
The descriptive information of the participants is shown in Table 1. We included individuals aged 18‒40 years; who were nonsmokers, who had full active movement of the neck, shoulder, or elbow; whose body mass index (BMI) was ˂30 kg/m2; and whose arterial blood pressure was normal (normotensive blood pressure: ˂135/85 mmHg). A history of upper extremity, cervical or thoracic fracture and surgery; a systemic musculoskeletal disease, pain in the neck and upper extremities; chest deformity and scoliosis; a history of deep vein thrombosis and embolism; regularly doing sports that involve overhead activity (i.e. tennis); doing regular elbow strength and other types of exercise for the last 6 months; being diagnosed with chronic diseases such as hypertension, peripheral vascular disease, and cognitive dysfunction were our exclusion criteria. All procedures were in accordance with the latest version of the Declaration of Helsinki and were approved by the ethical committee of XXXX University (Number/Date: XXXXX). All participants provided written and oral informed consent.
Table 1 Participant characteristicsInstruments
The primary outcome measurement was muscle strength. We measured elbow muscle strength while the participants were in the supine position, with a neutral shoulder, elbow 90˚ flexion, and forearm in supination for elbow flexion and in neutral for the elbow extension test. Stabilization was achieved by being held onto the upper part of the humerus. At the end range, we placed a hand-held dynamometer (HHD) (MicroFET®3; Hoggan Inc, UT, USA) just proximal to the medial and lateral styloid processes to test the flexors and extensors, respectively. We asked the participants to perform a gradually increasing maximum voluntary contraction in 2 s (until their effort matched that of the examiner) and then maintain it for 5 s. Three test results were averaged. We allowed a rest period of 20 s between repetitions and 1 min between tests [21]. On the basis of the test-retest results for 10 participants, our reliability was [ICC(3, k)] ICCflex=0.92, ICCext=0.96.
Secondary outcome measurements were proprioception and functional motor performance. For all JPS measurements, the absolute value of the difference between the target angle and the angle where the participant stopped was recorded. We allowed a rest period of 10 s between repetitions and 1 min between tests [22]. The use of a bubble inclinometer (Baseline®, Fabrication End Inc, NY, USA) shoulder JPS (A) for 100° shoulder elevation in the scapular plane was evaluated while the participant was sitting on a chair, (B) for 45° internal rotation (IR) and 75° external rotation (ER) while the participant was lying supine. In the rotation test, the elbow was at 90° flexion, the shoulder was at 90° abduction, and the participant’s palm indicated the face. The IR test ranged from 90° ER to 45° IR. The ER test ranged from the neutral position to 75° ER. The test positions were taught to the participants 3 times (when the target angle was reached, the participants held their arms for 3 s and then returned to the starting position), and afterward, they were asked to match the target angle 3 times (the results were averaged) [23] (ICCABD=0.78, ICCER =0.70, ICCIR=0.70.) For elbow JPS measurement, the participants sat on the chair with their backs supported and their hips flexed approximately 90°. The forearm was placed on the arms of the chair, covered with a foam pad, in a semi-prone position with the elbow fully extended at the starting position. The participants bent their elbow to the target angle (45°, 60°, and 75° flexion) controlled with a digital inclinometer (Baseline®, Fabrication End Inc, NY, USA), maintained this position for 5 s to learn the angle, returned to the initial position, and rested for 5 s. The protocol was repeated 3 times while their eyes were open and closed. In the actual test, we applied the same protocol 3 times (eyes were closed) and recorded the deviation from the target angle (the results were averaged) [22] (ICC45°=0.84, ICC60°= 0.89, and ICC75°=0.78).
The functional motor performance tests used in this study are the up-to-date, reliable, and essential assessment tools for upper extremity musculoskeletal/sports injury prevention, screening and return to sport after injury. They allow for a comprehensive evaluation of upper extremity function by emphasizing different aspects of performance [24,25,26]. All performance tests started with a warm-up activity from submaximal to maximal. For a high intensity effort, we verbally encouraged the participants throughout the tests. The tests were repeated 3 times, and the scores were averaged. We allowed a 45-sec rest period between repetitions in individual tests. The rest period was 60 s between tests [24]. The closed kinetic chain upper extremity stabilization test (CKCUEST) is used to assess upper extremity neuromuscular dynamic stability, strength, and endurance. In this test, we marked 2 lines (width = 3.8 cm) parallel to each other at a distance of 90 cm on a floor. The starting position for the test is one hand on each line while the body is in a pushup position. The participant moved both hands back and forth from each line as many times as possible in 15 s. Men were in the push-up position and women were in the modified push-up position (kneeling). The average number of lines touched, the score, and power were recorded (ICC = 0.87) [Score = (average of the number of lines touched / height), power = (68% weight * average number of lines touched) / 15] [27]. The modified pull-up test (MPUT) assesses an individual’s ability to perform movements which are essential for various sports and functional activities, strength, and endurance. Moreover, activity performed in the MPUT closely resembles the elbow flexion exercise, which is the primary exercise in the present research. The test was performed while the participants were positioned on their backs. We adjusted the metal frame above the head to be just above the shoulder level. Men perform the pull-up test with the support from their heels, and women perform the test with a step just below their knees [24]. To perform the test at full range, the participants started the test by holding the metal frame with their arms in full extension, pulling it parallel to the floor, and finally lowering their bodies with their elbows fully extended. During the test, we warned the participants to limit the movement of the head and trunk and to maintain the smoothness as much as possible. The participants performed the test with as many pulls as possible within 15 s during the 3 maximal tests (ICC = 0.85) [24]. The single arm shot put test (SASPT) is used to assess upper extremity power, strength, and coordination. The test was performed while the participants were seated in a chair with no arm support, with yellow tape affixed to the chair’s front legs, and the participant’s body was fixed to the chair via a velcro belt. The participants extended their legs to another chair so that their hips, knees, and ankles were in a straight line and parallel to the floor. The nonthrowing arm was placed on the opposite shoulder and a 3 kg medicine ball was launched from chest distance. We gave them 2 min rest after 4 warm-up shots with 25, 50, 75, and 100% effort from submaximal to maximum. Three maximal efforts were tested. The closest point and midpoint of the mark that the ball left when it touched the ground were measured in cm from the appropriate point of the tape affixed to the front legs of the chair (ICC = 0.98) [24]. Finally, we determined the functional throwing performance index (FTPI). The FTPI is an objective assessment tool used to evaluate upper extremity accuracy, power, consistency, and coordination. The test was performed by a 50.8 cm plastic ball that was thrown into a square area drawn on the wall which was 1.22 m above the ground and its edge width was 30.48 cm. The shooting distance from the wall was 4.57 m. First, the participants performed 4 controlled warm-up throws from submaximal to maximal. For testing, participants made a controlled maximum number of accurate throws in 30 s (FTPI = Number of shots within the target / Total number of shots * 100) (ICC = 0.79) [27].
Exercise protocol
The exercise was performed in a total of 75 repetitions, with the first set being 30 repetitions followed by 3 sets of 15 repetitions. A 30-sec rest was given between sets [28]. The exercise rhythm was determined via a metronome and the duration of contraction was set to 2 s for concentric contraction and 2 s for eccentric contraction. 1 RM was calculated using free weights. Free weights of 4 kg, 6 kg, or 8 kg were used according to the physical appearance of the individual. The number of repetitions they were able to lift in the relevant position was measured. Then, via the Holten diagram, a kg value equivalent to 20% of 1 RM was calculated. The elastic exercise band (Theraband, The Hygenic Corporation, ABD) was selected by considering the equivalent of kg in the elastic band force table. Since 20% of 1 RM does not always have the exact equivalent in the elastic band force table, a 10–30% range of 1 RM was taken into account, as suggested [29, 30]. In the first 4 weeks, exercise progression was achieved by increasing the pressure of the BFR cuff, whereas in weeks 5 and 6, exercise progression was achieved by changing the color of the elastic band. Elastic band color progressed so that ratings of perceived exertion during exercise ranged from 7 to 9 according to the OMNI Perceived Exertion Scale for Resistance Exercise with Elastic Bands (OMNI-RES EB) [31] Pain during exercise was less than “2” according to the numerical rating scale. The participants sat in a chair for the elbow flexion exercise, and the angle of the elbow joint during the exercise was adjusted in flexion from approximately 45˚-140˚ [30]. The BFR pressure band (cuff) (B Strong, Park City, Utah, ABD) was attached to the uppermost part of the arm. The pressure of the BFR cuff was maintained throughout the exercise. The pressure was adjusted to 80 mmHg in the first week, 90 mmHg in the second week, 100 mmHg in the third week, and 120 mmHg in the fourth week [31]. When starting each exercise session, the pressure was first set at 40 (± 5) mmHg and gradually increased to the desired pressure of the relevant week to avoid sudden pressure increase [31]. During the fifth and sixth weeks, the cuff pressure was 120 mmHg [9, 31]. After a careful review of previous studies’ protocols [9, 28, 30,31,32], this restriction pressure was selected because our population was not familiar with the technique and because excessive cuff pressure may augment the cardiovascular response, induce discomfort, and have negative effects on the sensorimotor system [2].
Control protocol
Controls received an educational brochure on the effects of exercise on different systems in the human body and its importance for health and protection from injuries. We asked them not to start any exercise program during the study and not to change their daily life routines, and we monitored their compliance by phone weekly.
Statistical analysis
We used SPSS v24.0 (IBM Corporation, NY, USA)” for data analyses. We determined the normality of the distribution of continuous data via the Shapiro-Wilk Test. We used the independent samples t-test to compare height, body weight, BMI, and age, and χ2 test to compare the sex and dominant extremity distributions of the groups. Two-way ANOVA [2 × 2, group (between-participant) x time (within-participant), repeated measures] was used to determine the intervention effects on the dependent variables. The F value was used based on sphericity assumed. We considered the time-group interaction term in the analyses. Between-group differences at the end of the intervention were also investigated. Pairwise comparisons were used to determine differences from the baseline to the completion of the intervention between groups and investigate whether any between-group differences in change scores were statistically significant. For nonnormally distributed data, we used the Wilcoxon signed-rank test to examine the changes in individual groups for the relevant results and the Mann-Whitney U Test to compare changes between two-time intervals between the groups. The significance level was p < 0.05.