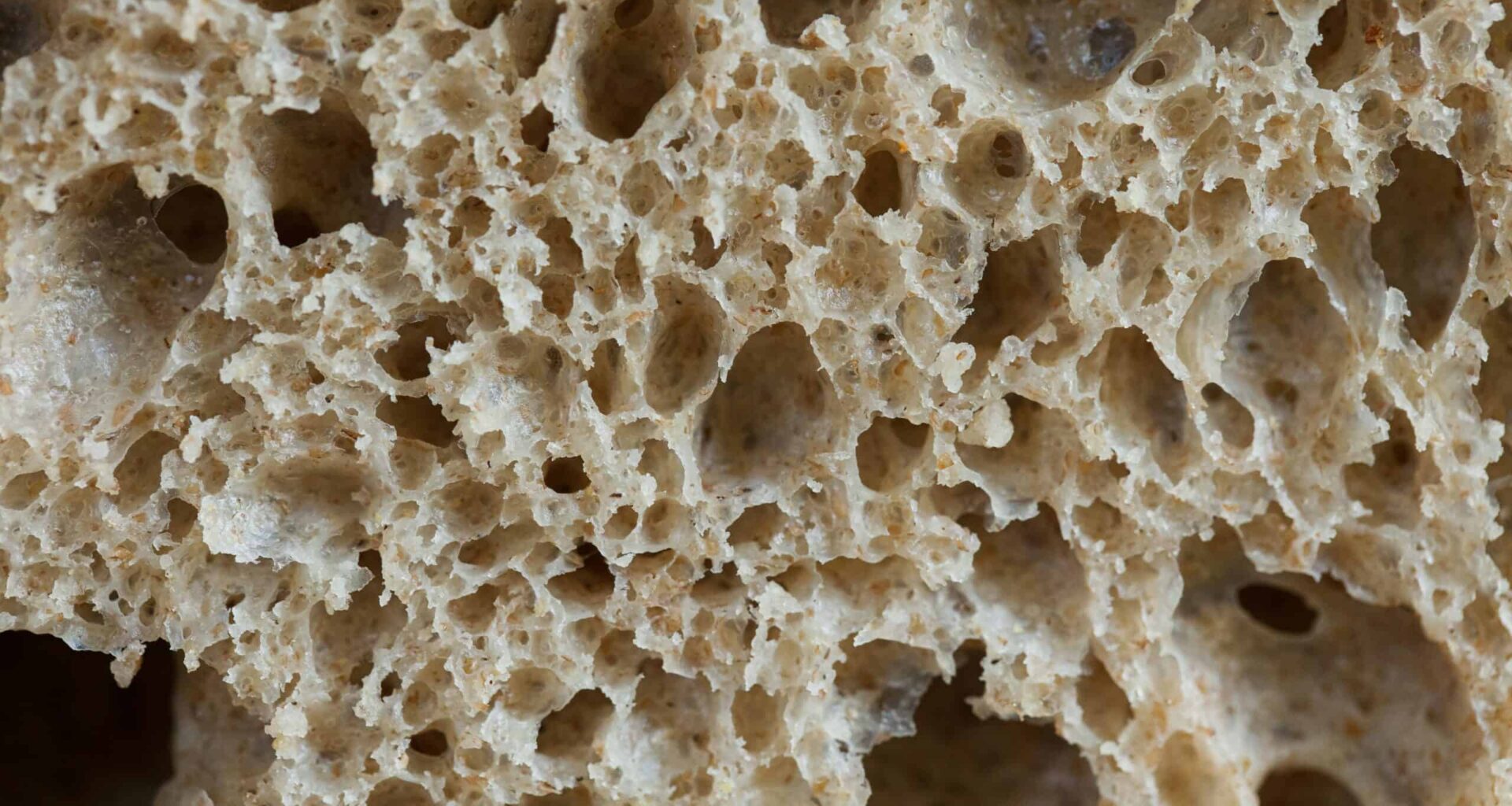
Bread may not be a big culprit. Image via Unsplash.
Bread may not be a big culprit. Image via Unsplash.
Millions of people around the world believe they have some form of gluten intolerance. Many cut gluten from their diet, sometimes going to great lengths to ensure this.
Associate Professor Jessica Biesiekierski from the University of Melbourne thinks many of them don’t need to do that.
Biesiekierski is an author of a major new review published in The Lancet. They found that that non-coeliac gluten sensitivity (NCGS), a condition that affects up to 13% of adults globally, is often not triggered by gluten at all. Instead, fermentable carbohydrates, other wheat components, or the brain’s interpretation of gut signals are more likely to cause the symptoms.
“Contrary to popular belief, most people with NCGS aren’t reacting to gluten,” said Dr. Biesiekierski in a university press release. “Our findings show that symptoms are more often triggered by fermentable carbohydrates, commonly known as FODMAPs, by other wheat components or by people’s expectations and prior experiences with food.”
Gluten Misunderstood
It’s always difficult to draw a conclusion when it comes to our diet because there are so many factors that could play a role. In the new study, researchers
The research team analyzed more than 58 studies investigating what really drives symptoms in people who say they are sensitive to gluten. Their findings were striking.
People with sensitive guts often experience gas and bloating after consuming fermentable carbohydrates found in onions, garlic, legumes, and certain fruits. The same applies to fructans, a specific type of FODMAP found in wheat, which researchers identified as a more likely trigger of symptoms than gluten itself.
The new review offers a striking contrast to the cultural narrative around gluten, which has been vilified in lifestyle magazines and by celebrities who claim gluten-free living is the secret to better health. But in tightly controlled clinical trials, something unusual happened.
“Across recent studies, people with IBS who believe they’re gluten-sensitive react similarly to gluten, wheat, and placebo,” Biesiekierski explained. “This suggests that how people anticipate and interpret gut sensations can strongly influence their symptoms.”
A Gut Feeling
That influence is part of a growing body of science exploring the gut–brain axis—the two-way communication system between the digestive tract and the central nervous system. One of the most revealing patterns in the studies reviewed was the power of the nocebo effect (like a placebo effect but negative). Participants who expected to feel unwell after eating gluten still developed symptoms, even without consuming it.
“These are real physiological responses,” the study’s authors wrote in The Conversation. “What the evidence is telling us is that focusing attention on the gut, coupled with anxiety about symptoms or repeated negative experiences with food, has real effects.”
In other words, the gut interprets signals through a lens of past experiences and emotional state. The result: normal digestion can feel like discomfort, urgency, or even pain.
This places NCGS on the same spectrum as irritable bowel syndrome, a disorder increasingly understood as a dysfunction in how the gut and brain communicate.
“Taken together, this redefines NCGS as part of the gut–brain interaction spectrum, closer to conditions like irritable bowel syndrome, rather than a distinct gluten disorder,” Biesiekierski said.
Is Gluten Ever to Blame?
 Gluten-free aisle. Credit: Wikimedia Commons
Gluten-free aisle. Credit: Wikimedia Commons
Yes. This study absolutely doesn’t negative that people with real gluten intolerance exist. But it’s far more rare than people assume.
Meta-analyses included in the review suggest that only about 16–30% of self-identified gluten-sensitive individuals actually experience gluten-specific symptoms under controlled testing. That’s a fraction of the estimated 10–15% of adults worldwide who believe they’re gluten sensitive.
Coeliac disease remains a very real autoimmune condition affecting around 1% of the population. For those individuals, gluten triggers immune damage to the gut lining, and avoiding gluten for life is essential.
This is all the more important because gluten-free alternatives tend to be more expensive and sometimes, less healthy than their counterparts.
“Gluten-free foods are, on average, 139% more expensive than standard ones,” noted the study authors. “They are also often lower in fibre and key nutrients.”
“Millions of people around the world avoid gluten believing it harms their gut, often after experiencing real symptoms that range from mild discomfort to severe distress,” Biesiekierski said. “Improving our scientific and clinical understanding of a condition affecting up to 15 per cent of the global population is incredibly important.”
Rather than defaulting to gluten-free living, the researchers propose combining dietary changes with psychological support, such as cognitive-behavioral therapy, to reduce food-related fear and reintroduce foods safely.
The researchers emphasize the need for improved diagnostic methods, clearer clinical guidelines, and more accurate public messaging. They urge clinicians to take patients’ symptoms seriously, even when gluten isn’t the underlying cause.
“Recognising this psychological contribution doesn’t mean symptoms are imagined,” the authors write. “When the brain predicts a meal may cause harm, gut sensory pathways amplify every cramp or sensation of discomfort, creating genuine distress.”