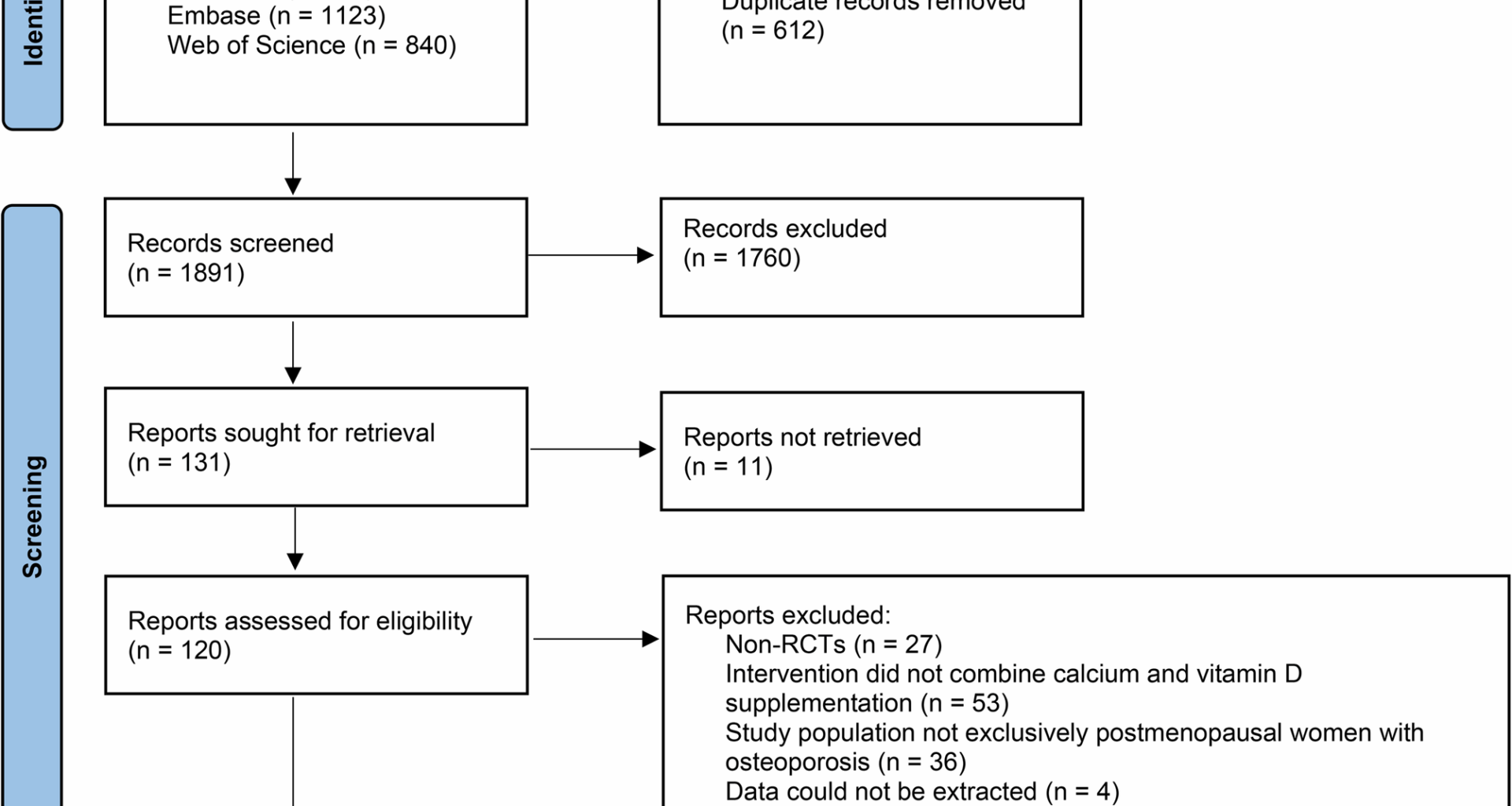
A total of 2503 documents were retrieved in PubMed, Web of Science, Embase and Cochrane Library. After screening, a total of 11 relevant documents were included, as shown in Fig. 1 for details [9,10,11,12,13,14,15,16,17,18,19].
Reference screening flow chart
Study characteristics
A total of 43,869 research subjects were included in 11 studies from 2005 to 2022, including 21,618 in the intervention group and 22,251 in the control group. The duration of intervention for patients spanned a wide range, with longer intervention lasting more than 10 years and shorter intervention lasting only 6 weeks. Of the studies with data, baseline serum 25OHD concentrations were severely deficient (< 25 nmolL − 1) in both groups of patients except one study. The control group of 2 studies had deficient baseline serum 25OHD concentrations (< 50 nmolL − 1), while the intervention group had normal baseline serum 25OHD concentrations (> 50 nmolL − 1). The baseline serum 25OHD concentrations of patients in both groups of another 2 studies were normal, and the remaining studies did not report baseline serum 25OHD concentrations. Patients in the intervention group of 3 studies did not use common calcium supplements and vitamin D supplements, but used dairy alternatives, including milk, yogurt, and cheese. Detailed characteristics are shown in Table 1.
Table 1 Characteristics of included referencesQuality of studies
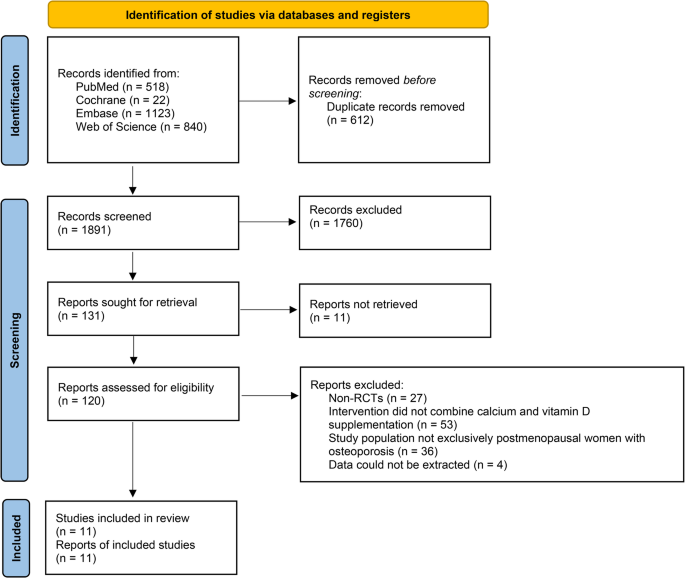
The risk of bias of the included studies was shown in Fig. 2. All studies were blinded with random sequence generation and had a low risk of bias. Six studies had a low risk of bias in allocation concealment, and the remaining studies had an unclear risk of bias. In terms of blinding of participants and staff, 4 studies had a low risk of bias, 2 studies had an unclear risk, and 5 studies had a high risk. The outcome assessment risk of bias was low in 9 studies and unclear in the remaining studies. Due to incomplete outcome data, 9 studies had a low risk of bias and the remainder had an unclear risk of bias. The risk of bias in selective reporting was unclear in only 1 study, and the risk of bias in the remaining studies was low. Other biases were low in 4 studies and unclear in the remaining studies.
Literature quality evaluation
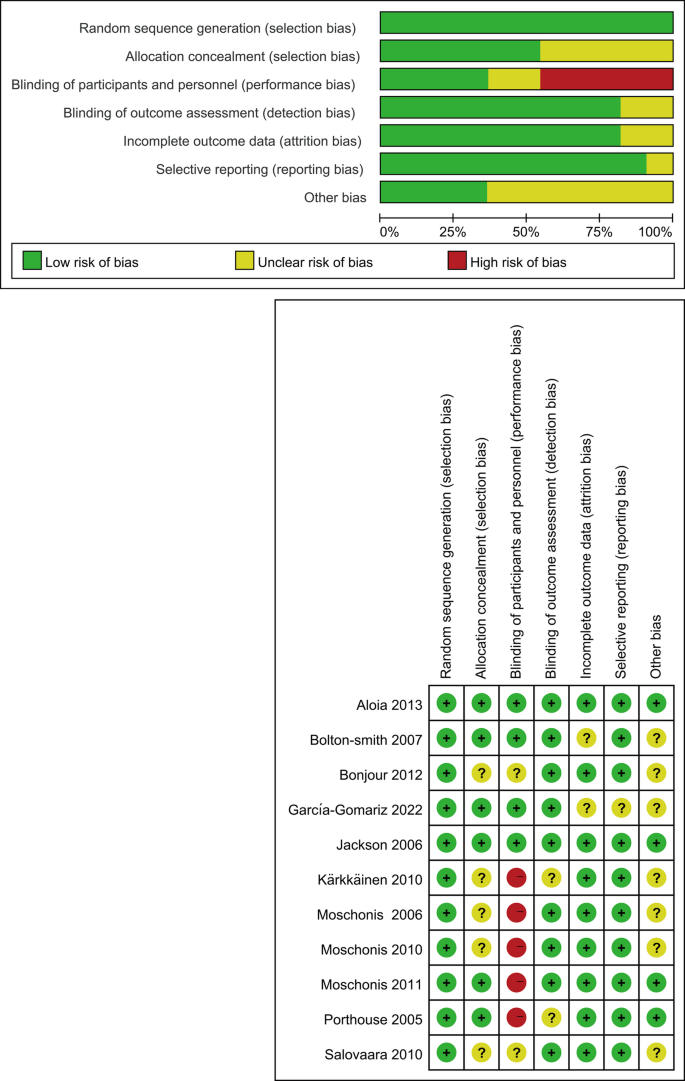
Effects of combined calcium and vitamin D intervention on BMD in postmenopausal women
Four studies analyzed the effect of combined calcium and vitamin D intervention on systemic BMD in postmenopausal women. Although the results showed that the BMD of patients in the intervention group was improved compared with the control group, the effect of combined medication on BMD in postmenopausal women was not significant (Z = 1.80, P = 0.07). Heterogeneity analysis showed that the study results were moderately heterogeneous (I2 = 59%) (Fig. 3A, Figure S1 A). Two studies reported the effect of combined calcium and vitamin D intervention on arm BMD in menopausal women. The results showed that there was no significant difference between the intervention and the control (Z = 0.93, P = 0.35), and the heterogeneity was high (I² = 78%) (Fig. 3B, Figure S1 B). Two studies reported the effect of combined calcium and vitamin D intervention on tibial BMD in menopausal women. The results showed that there was no significant difference between the intervention and the control (Z = 0.19, P = 0.85), but the heterogeneity was very low (I² = 0%) (Fig. 3C, Figure S1 C), which indicates that the difference between the results of the two studies is small. For lumbar spine L2-L4 BMD, two studies reported this part, but the difference between groups was not significant (Z = 0.83, P = 0.41) and the heterogeneity was low (I² = 0%) (Fig. 3D, Figure S1 D). It was worth noting that in the analysis of pelvic BMD, a meta-analysis of data from the intervention and control groups of the two studies showed that the combined intervention of calcium and vitamin D significantly enhanced pelvic BMD in women after terminal illness (Z = 2.13, P = 0.03), and heterogeneity analysis showed high consistency between study results (I² = 0%) (Fig. 3E, Figure S1 E). In addition, two studies reported the effects of combined calcium and vitamin D intervention on biochemical markers of bone resorption in postmenopausal women, such as serum C‑terminal telopeptide of type I collagen (CTX), Calcium‑to‑creatinine ratio (Ca/Cr), and TRAP 5b. Aloia et al. [17] showed that serum CTX levels remained more stable in the intervention group compared with the control group. There were no significant differences in changes in serum Ca/Cr and TRAP 5b between the two groups. In addition, García-Gomariz and colleagues [19] believe that moderate exercise when combined with calcium and vitamin D can better improve bone density in postmenopausal women.
Effect of combined calcium and vitamin D intervention on bone density in postmenopausal women. A Whole body BMD; (B) Arm BMD; (C) Tibia BMD; (D) Lumbar spine L2-L4 BMD; (E) pelvic BMD
Effects of combined calcium and vitamin D intervention on 25OHD in postmenopausal women
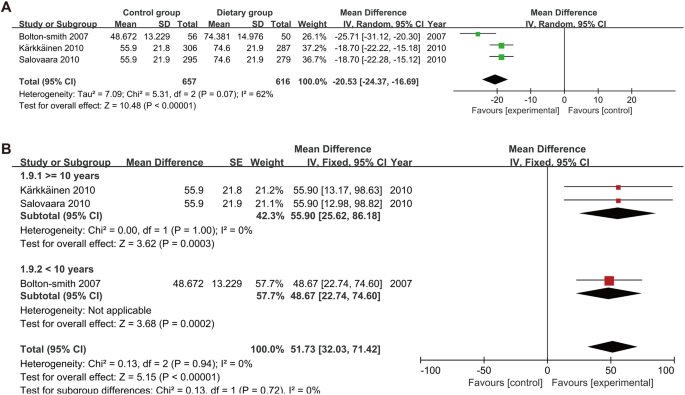
Three articles recorded the changes in 25OHD levels in patients after combined treatment with calcium and vitamins. The results showed that compared with the control group, the 25OHD levels in patients after combined treatment were significantly increased (Z = 10.48, P < 0.001). Heterogeneity was moderate (I² = 62%) (Fig. 4A, Figure S1 F). In addition, we found that in a group of patients with severe deficiencies in serum 25OHD concentrations at baseline, serum 25OHD concentrations in control patients did not return to normal levels after the end of the trial. In the other two control groups, the serum 25OHD concentration returned to normal levels in patients with baseline deficient serum 25OHD concentrations. We conducted a subgroup analysis based on the patient’s supplementation duration, and the results showed that the supplementation duration was not a factor affecting the patient’s serum 25OHD concentration (P = 0.72), and the heterogeneity between studies was low (I² = 0%) (Fig. 4B, Figure S1 G).
Effect of combined calcium and vitamin D intervention on 25OHD in postmenopausal women. A 25OHD; (B) Subgroup analysis of the impact of intervention time on 25OHD
Effect of combined calcium and vitamin D on incidence of fractures in postmenopausal women
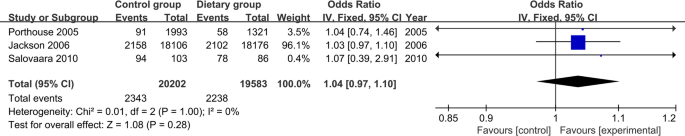
Fracture outcomes were reported in three RCTs encompassing 42,000 + postmenopausal women. In the Women’s Health Initiative (WHI) trial, supplementation with 1000 mg elemental calcium plus 400 IU vitamin D3 daily for a mean 7.0 years produced hazard ratios (HRs) of 0.88 (95% CI 0.72–1.08) for hip fracture and 0.96 (0.91–1.02) for total clinical fractures, indicating no statistically significant reduction versus placebo [14]. In the primary‑care trial of women aged ≥ 70 years with ≥ 1 hip‑fracture risk factor, daily 1000 mg calcium plus 800 IU vitamin D3 did not reduce all clinical fractures (adjusted odds ratio [OR] 1.01; 95% CI 0.71–1.43); the OR for hip fracture was 0.75 (0.31–1.78), also non‑significant [15]. Similarly, in the 3‑year The Osteoporosis Risk Factor and Prevention Fracture Prevention Study (OSTPRE‑FPS) population study of 65‑ to 71‑year‑old women, daily 1000 mg calcium plus 800 IU vitamin D3 yielded an adjusted HR of 0.83 (95% CI 0.61–1.12) for any fracture, which was not statistically significant compared with controls [9]. Pooled analysis across these three trials showed that the combination of calcium and vitamin D did not reduce the incidence of total fractures in postmenopausal women (Z = 1.08, P = 0.28). Heterogeneity analysis showed high agreement between study results (I² = 0%) (Fig. 5, Figure S1 H).
Effect of combined calcium and vitamin D intervention on fractures in postmenopausal women
Sensitivity analysis and publication bias
Our qualitative assessment did not indicate significant publication bias. The results across studies were consistent, with no evidence suggesting a systematic overrepresentation or underrepresentation of study findings. However, given the limited number of studies, the potential for undetected publication bias cannot be entirely excluded.