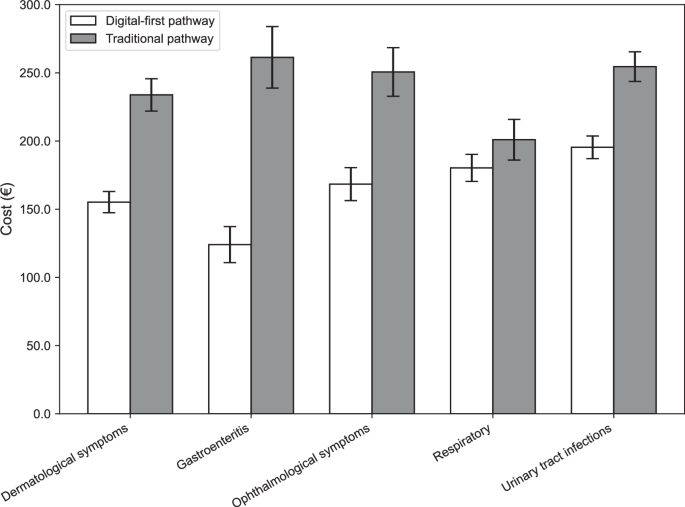
In our study setting common minor acute primary care episodes initiated via a digital-first pathway were associated with approximately 23% lower costs on average compared to traditional pathways, without increasing follow-up visits or diagnostic test usage. By analyzing 17 months of data from a Finnish primary care setting, we observed consistent cost reductions across multiple diagnostic categories. These findings reinforce prior research suggesting that digital health interventions could potentially generate economic benefits16.
The observed cost-effectiveness of the digital-first pathway is primarily driven by lower encounter costs. Chat-based digital care has the potential to reduce costs primarily through efficiency gains from the use of automated and standardized questionnaires and asynchronous communication (the same healthcare professional can evaluate multiple patients simultaneously). Our findings suggest that digital consultations are often sufficient for managing the examined conditions, with no observed increase in subsequent healthcare contacts compared to traditional pathways. Consequently, encounter costs in the digital-first pathway are substantially lower and account for the majority of observed cost savings (Table 3). Differences in laboratory testing and imaging utilization were present but contributed less significantly, underscoring that encounter costs are the primary driver of savings.
Moreover, our results suggest that fewer laboratory and imaging studies are ordered in digital-first pathways. Conservative testing practices are encouraged in the examined digital care model and management of common issues is more heavily standardized. Healthcare professionals may emphasize clinical history and adopt a watchful waiting approach for mild cases. In a traditional in-person setting clinicians may have a tendency to perform additional diagnostic tests as a precaution or to reassure the patient. Overuse of low-value diagnostics in traditional settings can contribute to increased healthcare expenditures, whereas digital health platforms may inherently promote more judicious resource utilization via stronger standardization of practices.
These findings contribute to the growing body of evidence on the effectiveness of digital consultations in primary care. Glock et al. demonstrated that eVisits in Swedish settings were suitable for managing uncomplicated conditions, with the majority of patients not requiring follow-up17. Likewise, studies focusing on minor acute illnesses have generally reported no increase in downstream utilization following digital encounters18,19,20,21,22,23, with some reporting reduced service use24. However, earlier investigations have also noted increased follow-up visits and higher healthcare utilization following digital encounters8,25,26,27,28, particularly in cases of acute respiratory tract infections29. While few studies have assessed costs directly, those that have typically suggest favorable economic outcomes5. One exception is the study by Ashwood et al.30 which found higher costs for digital consultations in respiratory cases. Notably, respiratory infections represented the only diagnostic category in our study with increased follow-up rates and the smallest relative cost savings.
The magnitude of cost savings in our study, ranging from 20 to 50% depending on condition, is higher than previously reported in some settings. For example, Buvik et al. observed a 19% cost reduction in orthopedic teleconsultations, contingent upon sufficient patient volume31. Gentili et al. found that over half of the studies in their review reported digital interventions as dominant – both more effective and less costly5. Ayabakan et al. similarly reported a 13.6% reduction in future outpatient visits and $239 in cost savings within 30 days of a telehealth encounter, with the strongest effects observed in conditions amenable to virtualization, such as mental health, skin, metabolic and musculoskeletal diseases32. On the other hand, a scoping review in Australia cautioned that telehealth’s system-wide savings were not always realized because of how services were funded and organized33. Importantly, our study setting enabled digital consultations to function as true substitutes. The digital platform is integrated with clinical infrastructure, allowing for laboratory orders, referrals, and escalation to in-person visits when necessary. This integration is critical – if digital services merely add another layer of care, overall utilization and costs may increase. In our context, where the same provider organization managed both digital and traditional services, care was coordinated to avoid unnecessary steps or layers. In our study digital encounters did not result in excess follow-ups, reinforcing the role of digital care as a substitute rather than a supplement.
These results have meaningful implications for healthcare policy. Scaling digital-first care models, particularly for conditions shown to be safely manageable online, may offer a viable strategy for health systems seeking cost savings. Importantly, these savings do not require workforce reductions but could instead alleviate pressure to scale staffing proportionally with rising care demands – particularly as populations age and service needs increase. However, careful attention to clinical quality and health equity is warranted. Digital care protocols must include safeguards such as appropriate triage and escalation of care. Quality monitoring mechanisms are essential to ensure that cost reductions do not compromise clinical outcomes.
Another major implication is the need to address the digital divide. Our findings highlight a considerable age disparity in digital-first pathway utilization, with younger patients disproportionately using digital healthcare services. This aligns with prior evidence suggesting that older adults, individuals with limited internet access, and those with lower digital literacy are less likely to engage with digital health solutions7,8. Additional barriers may also affect individuals with cognitive impairments or language difficulties. If these disparities remain unaddressed, the benefits of digital healthcare – such as improved access, convenience, and cost savings – may be inequitably distributed, reinforcing existing healthcare inequalities.
However, digital health also has the potential to enhance accessibility, particularly in remote or underserved regions where traditional healthcare infrastructure is limited34,35. In the studied time period virtually all mobile phone plans in Finland include internet access, with full coverage of the geographical area. Additionally, patient fees for digital and traditional consultations are comparable, typically zero euros when only the initial contact is involved, suggesting that financial barriers are unlikely to explain differences in uptake. Nonetheless, disparities persist in digital engagement, as not all individuals are willing or able to use digital services. To ensure equitable adoption, targeted interventions should be implemented, including digital literacy programs tailored to older populations, and user-friendly app designs that accommodate a wide range of technological proficiencies. Moreover, successful integration of digital care could free up resources for patients preferring the traditional settings, potentially improving access outside digital care.
Our results also feed into the broader discussion of healthcare system reform. Finland’s healthcare reform seeks cost savings to rein in deficits, and digital health has been highlighted as a key strategy. The results from this study supports those strategic directions – a digital-first primary care model could indeed contribute to cost containment in the region. Policymakers and administrators can leverage these findings to justify investments in digital platforms. While there is an upfront cost to building and maintaining apps and IT infrastructure, the return on investment appears favorable given the per-episode savings. Additionally, while our analysis focused on the provider’s perspective, other benefits such as reduced transportation costs, lower absenteeism, patient preference36,37,38,39 and reduced emissions40,41 further strengthen the case for digital-first pathways, even though these were not quantified in this study.
This study has several limitations to acknowledge. First, despite propensity score matching, residual confounding may bias the estimates. Unmeasured factors – such as clinical complexity, digital literacy, patient preference or provider differences – may have influenced both care pathway selection and costs. As illustrated in Supplementary Figs. 1 and 2, patients appear to favor the same modality for follow-up visits, suggesting that patient preference may play a role. This may introduce behavioral confounding, such as self-selection into digital or in-person encounters. Furthermore, physicians in the digital clinic are compensated on an hourly basis, whereas their in-person counterparts receive fixed monthly salaries. This difference in payment structure could potentially influence clinical engagement and decision-making incentives. Additionally, some differences in prescribed medications remained between groups after matching, reflecting in part differences in case-mix and differences in clinical management (Supplementary Tables 9 and 10). Nonetheless, the observed cost differences were substantial, making it unlikely that residual confounding alone explains the findings.
Second, as a cost-minimization analysis, we did not directly assess clinical outcomes such as symptom resolution, patient satisfaction, or complication rates. We assumed equivalent outcomes between pathways based on clinical judgment and similar follow-up rates (Table 2). We did not attempt to assess differences in clinical outcomes due to limited statistical power, since outcomes reliably ascertainable via available registry data are rare (e.g. hospitalization due to pneumonia). While prior studies suggest that telemedicine provides comparable outcomes for common acute conditions, differences in quality or patient outcomes cannot be ruled out.
Third, our findings are limited to acute, low-complexity conditions commonly managed in primary care. This analysis therefore excludes inpatient encounters. This may lead to an underestimation of total costs in episodes involving hospital care, although such events are expected to be rare given the low-acuity nature of the conditions studied. Furthermore, results may not generalize to clinical presentations we did not study, for example management of chronic illnesses in multimorbid patients, mental health or primary prevention. Evaluating the cost and clinical performance of digital-first care for these populations remains an important area for future research.
Fourth, the study is region-specific, focusing on Päijät-Häme in Finland, within a healthcare system that integrates digital services into public primary care. The digital clinic provides quick access to care, with extensive opening hours, typically with a low waiting time of less than 15 minutes, and virtual clinicians have the same capabilities as phone-based services for scheduling appointments and issuing referrals. The region also maintains strong access to in-person care, with acute appointments frequently available on the same day. While the findings are likely generalizable to settings with similar infrastructure and care models, their applicability to healthcare systems with different payment structures – such as purely fee-for-service models – is uncertain. Differences in reimbursement incentives, physician practice patterns, patient digital literacy, and clinician acceptance may all influence care processes and outcomes, potentially limiting the transferability of our results to other healthcare environments.
Fifth, the time horizon was relatively short (14 days, with a 7-day and 30-day sensitivity analyses), capturing only the associated acute episode costs. While this timeframe is appropriate for evaluating short-term healthcare expenditures17, it does not account for any potential long-term cost implications. We chose a relatively short time horizon as the registry data does not allow separation of related and unrelated costs, consequently the longer the horizon, the more it is contaminated by unrelated costs. If digital consultations led to increased downstream healthcare utilization beyond the 30 days, such effects would not be captured in this analysis. Both the supplementary analysis of follow-up care (Supplementary Fig. 3) and the 30-day cost sensitivity analysis (Supplementary Table 6) suggest that cost savings observed for digital-first care were not offset by increased resource use later in the care pathway. Nonetheless, longer-term studies are warranted, particularly to assess the economic impact of digital-first pathways for chronic disease management.
Sixth, cost estimates are inherently subject to variability. Our analysis is based on publicly available regional cost data, which represents average production costs rather than real-time, transaction-level expenditures. While this approach aligns with economic evaluation best practices, healthcare cost structures vary across systems, and the results may not fully capture hidden or indirect costs associated with digital-first and traditional pathways.
Seventh, episode-based costing may include services unrelated to the minor acute condition. However, this applies equally to both groups and is unlikely to introduce systematic bias.
Eight, the study examined costs solely from the healthcare provider’s perspective, excluding societal costs such as patient travel expenses, lost work time, or productivity losses. Given that digital consultations eliminate the need for physical travel and reduce time burdens for patients, incorporating these factors in future cost-benefit analyses would likely strengthen the case for digital-first pathways.
In summary, this study supports the view that digital-first primary care pathways could reduce healthcare costs for the examined common minor acute conditions in primary care without a significant increase in follow-up visits. In the examined Finnish healthcare system, digital-first pathways lowered the cost of managing common infections and minor illnesses by approximately 20-50%, depending on the condition. These findings support the integration of digital health solutions as a scalable strategy to improve efficiency in healthcare systems with similar structures.
However, achieving widespread adoption while ensuring equitable access and maintaining clinical quality will be critical. With thoughtful implementation, digital-first pathways may help ease pressure on rising healthcare expenditures, a key priority for the long-term sustainability of health systems globally.