We utilized chromosomal microarray analysis (CMA) and whole exome sequencing (WES) to investigate the prevalence of clinically relevant CNVs and SNVs/Indels in an unselected cohort of 101 CHD patients without clear etiology. we got a higher general prevalence of chromosomal abnormalities of 20.8% (21/101), which is consistent with a recent Chinese study that identified pathogenic/likely pathogenic CNVs in 24/104 (23.1%) CHD patients20confirming the important role for CMA in clinical settings. Among them, 26 individuals classified as non-isolated CHD when they had at least one extracardiac multiple congenital anomaly (MCA), such as craniofacial anomalies, neck anomalies, cleft palate, trachea and thorax abnormalities, hernia, genitourinary malformation and skeletal dysplasia as well as DD and ID. However, due to younger age, lack of certain clinical manifestations and inadequate clinical assessment, it is possible to classify the two groups of isolated and non-isolated patients inaccurately. For instance, Langer-Giedion syndrome is a rare chromosomal syndrome with deletions of the distal part of 8q24.1, characterized by distinct facial features, mental retardation, bone abnormalities and some patients suffering from CHD, which is hard to be recognized in childhood21. In our study, a 14.2 deletion at 8q24.11q24.22 was identified in a 1-month-12-day boy with complete atrioventricular septal defect, while no other phenotypes were noted when he was enrolled, so he was classified incorrectly into isolated CHD group.
We re-assessed retrospectively the clinical presentations of the patients with recognizable features of the identified genetic syndromes and compared with previously reported cases in the literature. For example, 22q11.2 deletions are among the most frequent genetic causes in individuals with CHD and present with a variety of clinical features. About 64% of individuals with 22q11.2 deletion syndrome have heart defects and > 90% are de novo22,23. Consistently, 5 cases in the study identified 22q11.2 deletion syndrome (DiGeorge syndrome) presented facial features (4/5), TOF/VSD (5/5), hypocalcemia (2/5), immunodeficiency (2/5), and DD (1/5) who were 4 de novo and 1 maternal inherited. Trisomy-21 (known as Down syndrome) is the most common chromosomal abnormality in CHD patients who usually have distinctive pattern of clinical features, such as global developmental delay, intellectual disability, characteristic face, microcephaly, and other physical traits so that it is generally do not require genetic testing for them to obtain a diagnosis and most studies investigating the yield of genetic testing in CHD patients exclude cases of trisomy-21 as these patients24. A 11-day-old boy with complete atrioventricular septal defect and mild craniofacial anomalies was identified as trisomy-21, but he was not recognizable before he was enrolled due to his young age and lack of distinctive features.
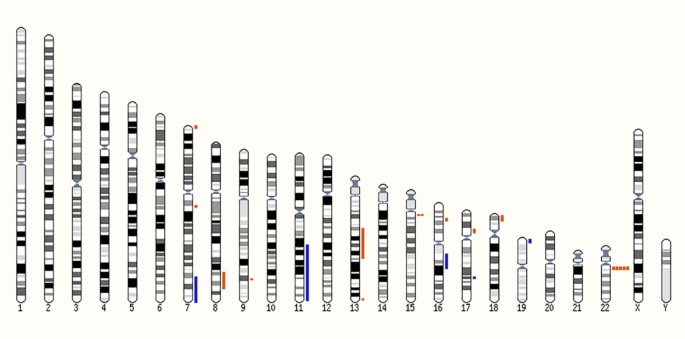
Interestingly, we detected 3 rare de novo CNVs at chromosome 7 in one 3-month-17-day-old boy with complex phenotypes of multiple systems such as perimembranous ventricular septal defect, agenesis of corpus callosum, scoliosis, hypotonia, microphallus, hypospadias, and DD. The 3 CNVs include a 1.8 Mb deletion at 7p22.3 encompassing 36 genes and a major OMIM gene of FAM20C (#611060). There are 6 individuals with overlapping deletions (from 1.12 Mb to 2.32 Mb) and a variety of phenotypes mainly including DD, ID, cognitive impairment and seizures in the DECIPHER database. The second CNVs, a 1.8 Mb duplication at 7p22.2 involving 19 genes has been associated with developmental delay, mild ID, asthma, myopia, dysmorphic features in the literature25. There are additional 21 cases with overlapping duplications (from 198.88 kb to 2.23 Mb) and a variety of phenotypes mainly including abnormal heart morphology, cerebellar vermis hypoplasia, renal hypoplasia, cognitive impairment, scoliosis, strabismus, and ID in the DECIPHER database. The third CNV is a 23.5 Mb duplication at 7q33q36.3 encompassing over 100 genes, overlapping reported however smaller microduplications of 507 kb, 730 kb and 1.35 Mb from 7q36.1 to 7q36.3. The 507 kb duplication at 7q36.3 was found in a 20w6d fetus with multiple congenital anomalies like cleft lip/palate, prominent cavum septum pellucidum, right-sided heart position, absent right radius and thumb, fixed right forearm, and scoliosis26; the 730 kb duplication at 7q36.3 was found in four individuals from a three-generation family with agenesis of the corpus callosum and mild ID, macrocephaly27; the 1.35 Mb duplication at 7q36.1q36.2 was found in a 22 month old child presenting with hypotonia, respiratory distress, feeding difficulties, cardiovascular malformation, growth failure with microcephaly, short stature, sensorineural hearing loss, myopia, cryptorchidism, hypospadias, microphallus, distinctive facial features and DD28. Furthermore, from the DECIPHER database additional 109 cases with duplications within 7q33q36.3 presented some overlapping manifestations, such as corpus callosum dysplasia, scoliosis, muscular hypotonia and microphallus, macrocephaly, cardiac defects, TOF, and ID. Likely, the 3 de novo CNVs could be a more complex structural rearrangement, such as a ring chromosome (often mosaic) which contribute to the phenotype of this individual, but more follow-up work is needed in the future.
Through WES, we identified ten pathogenic and likely pathogenic variants in 8 individuals, and most genes (including FLNA, KANSL1, TRAF7, KAT6A, PKD1L1, and RIT1) have previously been associated with syndromic CHD29,30,31,32,33,34. However, 4 genes of TRAF7, KAT6A, PKD1L1, and RIT1 were found in probands with isolated CHD. The main reason should also be clinically unrecognized associated features especially in young patients. Our findings provide further evidence supporting an important role of these genes in CHD. FLNA, located on chromosome Xq28, encodes an actin – binding protein (filamin A) expressed in virtually every tissue, and mutations in the FLNA gene cause X-linked filaminopathies including cardiovascular malformations, such as X-linked cardiac valvular dystrophy (CVDPX; OMIM#314400), X-linked periventricular nodular heterotopia (PVNH1; OMIM#300049), FG syndrome-2 (FGS2; OMIM#300321)35,36. We identified an exon 8–9 duplication in the FLNA gene in a 7-month- old boy (J102) presenting with perimembranous ventricular septal defect, trachea abnormality and umbilical hernia. He died at 10 months of respiratory insufficiency and heart failure. The intragene duplication was predicted to cause loss-of-function of the FLNA gene. Other individuals with loss-of-function variants in the FLNA gene presented with periventricular nodular heterotopia, heart defects, interstitial lung disease, respiratory failure, and/or early death, further indicating an association of FLNA deficiency and congenital malformations of the brain, heart and lungs37,38.
In this study, we performed sequential genetic testing using CMA followed by trio-WES in a cohort of unselected CHD patients in order to obtain reliable diagnostic yields. Our study indicates that trio-WES increments the diagnostic yield in patients with extracardiac features but also in those with apparently “isolated” CHD. It’s worthy noting that finding de novo pathogenic variants in genes with an uncertain link to CHD, does not prove this association but may contribute data to support this association. In addition, the sample size was small, and it is possible missing some dual diagnoses by only performing exome on the patients with negative CMAs, further studies with large samples and using genome sequencing are warranted to find new genes and variants, and to assess the clinical spectrum and recurrence risks in affected individuals and their families.